In April 2011, the EFNS together with ENS and ECTRIMS, have published this important statement. What is the follow-up?
https://www.efns.org/uploads/media/CCSVI_in_MS_ECTRIMS_EFNS_ENS_02.pdf
Chronic Cerebrospinal Venous Insufficiency (CCSVI) in Multiple Sclerosis – From “The Big Idea” to “The Perfect Crime”?
By Christos Krogias, on behalf of EFNS and ENS, Ruhr University Bochum, Germany
Michel Clanet, on behalf of ECTRIMS and ENS, University of Toulouse, France
Giancarlo Comi, on behalf of ENS, University Vita-Salute San Raffaele, Milan, Italy
Ralf Gold, on behalf of ECTRIMS and EFNS, Ruhr University Bochum, Germany
Gian Luigi Lenzi, on behalf of EFNS, University of Rome, Italy
Xavier Montalban, on behalf of ECTRIMS, University of Barcelona, Spain
Per Soelberg Sørensen, on behalf of ECTRIMSrand EFNS, University of Copenhagen, Denmark
Multiple sclerosis (MS) is a chronic, primarily inflammatory demyelinating disease of the central nervous system (Compston and Coles, 2008). Pathogenesis is triggered by environmental factors in combination with genetic susceptibility. Typically migration of autoreactive lymphocytes across the blood-brain barrier initiates the activation of a complex autoimmune cascade, where monocytes and microglial cells then step in and further augment tissue damage by oxidative mechanisms. The histological hallmark of the disease is a perivenous sclerotic plaque, characterised by inflammation, oligodendrocyte depletion, astrocytosis, de-and remyelination as well as subsequent axonal degeneration (Lucchinetti et al., 2000).
This perivenous formation of the plaque has set the stage to introduce the hypothesis that a venous blockade may stand at the beginning of the chronic autoimmune process and may thus represent the true pathogenetic cause of the disease. A putative venous congestion has been discussed as a contributing factor to the pathogenesis of MS already 30 years before (Allen, 1981).
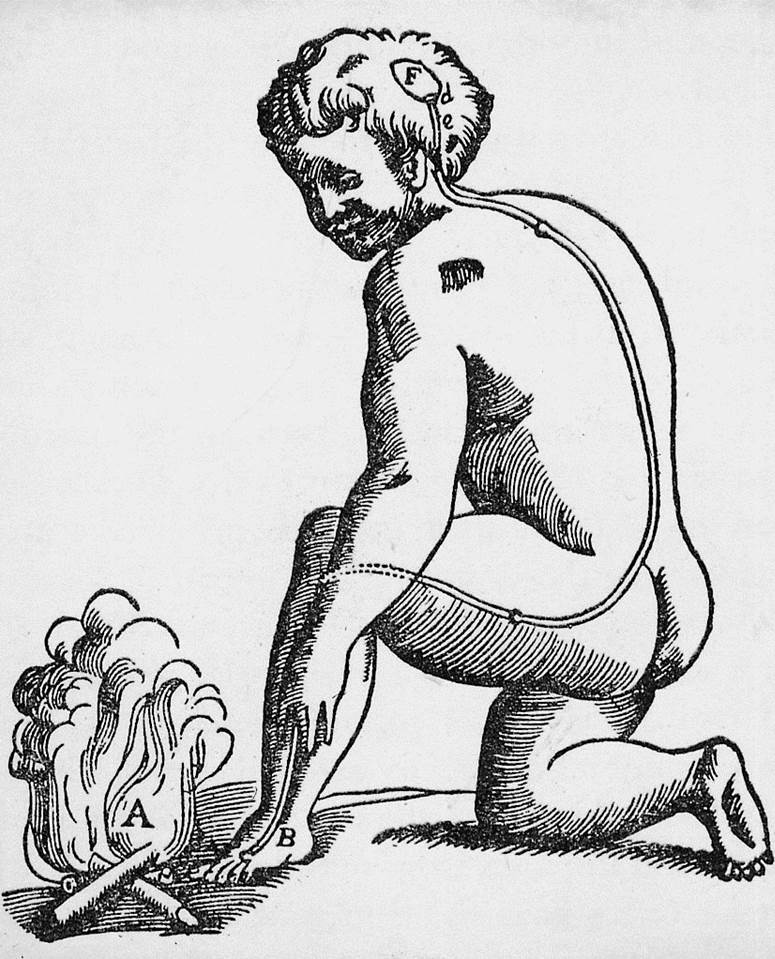
This discussion was resurrected in the year 2006 by Paolo Zamboni from Ferrara, Italy, who proposed parallels between an iron-dependent inflammation in chronic venous insufficiency (CVI) of the lower limbs and the perivenously located white-matter lesion in MS. He stated that his considerations may represent “The big idea” (Zamboni, 2006). Three years later, Zamboni et al. reported an impressive coincidence of MS and venous stenoses demonstrated with ultrasound investigations in various locations of deep cervical veins (Zamboni et al., 2009). This concept was then named “chronic cerebrospinal venous insufficiency” (CCSVI). In this concept it is hypothesized that a blockage of venous flow leads to an increased venous blood pressure in the central nervous system, which in turn causes congestional bleeding with perivenous iron accumulation and subsequent inflammatory reactions (Zamboni 2009a).
In considering CCSVI as a highly specific finding in MS, it should be remembered that cerebral venous insufficiencies were already discussed as a causal factor in other neurological diseases such as transient global amnesia or idiopathic intracranial hypertension (Schreiber et al., 2005; Nedelmann et al., 2009). Furthermore, other conditions such as neck-dissection surgery result in changed venous outflow (Gius and Grier, 1950).
There is no scientifically proven evidence for a higher incidence of MS in such patients with confirmed venous obstruction, so that serious doubts are raised about the conceptual plausibility of CCSVI as a significant factor. In addition, the spectacular findings of Zamboni et al., reporting not only a high specificity but also a high sensitivity of venous pathology in MS, could not be reproduced by other groups.
In a small cohort of unselected MS-patients and matched controls in Bochum, Germany, only two fulfilled the required neurosonological features of CCSVI (Krogias et al., 2010). The group of Doepp et al. (Berlin, Germany), having a large experience of venous neurosonography, performed an extended study protocol in 56 MS-patients. None fulfilled the criteria for CCSVI (Doepp et al. 2010). At the 2010 annual meeting of the AAN, Zivadinov et al. (Buffalo, USA) reported the presence of venous construction in more than 50% of MS patients, whilst CCSVI was also detected in about 30 % of the healthy controls (Zivadinov et al., 2010).
An Italian group from Padua (Baracchini et al., 2011) recently performed a very interesting study investigating 50 patients with a clinically isolated syndrome (CIS) and with additional evidence of dissemination in space of the inflammatory lesions (possible MS). In only eight (16%) of them were the CCSVI criteria fulfilled. In seven, additional selective phlebography was performed, revealing hypoplasia of internal jugular vein in one case as the only venous abnormality within the whole series. If CCSVI causes MS, one would expect the presence of CCSVI already at the onset of the disease. The findings of this Italian study do not support a causal relationship between CCSVI and MS.
These results are of special interest since Prof. Zamboni promotes endovascular intervention as a groundbreaking treatment of MS. An open-label trial was published by Zamboni et al. in the Journal of Vascular Surgery in 2009. In 65 patients with MS percutaneous transluminal rangioplasty (PTA) was performed (Zamboni et al., 2009b). Most of the patients were on disease-modifying therapies. There was a lack of a control group. The authors claimed that this procedure has led to an improvement of the clinical outcome in relapsing-remitting MS (RRMS) patients. Being aware about the high variability of MS disease course, the improvement described may reflect the natural outcome, as clinical relapses mostly show remission. The effect on the annual relapse rate was not different from that reported from placebo treatment in placebo-controlled clinical trials. In patients with progressive forms of the disease no improvement was observed after PTA. Zamboni self-proclaimed this intervention as “liberation procedurer”. Unfortunately, such a name raises inappropriate expectations among MS patients.
Recently, a third German group (Frankfurt/Giessen) performed a sonographic study investigating 20 MS patients and 20 controls (Mayer et al., 2011). The only subject fulfilling the CCSVI-criteria was a subject from the healthy control group. As these findings cast serious doubt on the concept of CCSVI in MS, the authors entitle appropriately their paper “The perfect crime? CCSVI not leaving a trace in MS”
Conclusion and recommendations: Based on these extensive, scientifically solid data obtained from investigators outside of Ferrara, we see no rationale to support CCSVI as a key pathogenetic factor in MS.
Furthermore an ongoing large multi-center Italian epidemiological study recruiting more than 1000 MS patients and about 1000 healthy controls and patients with other neurodegenerative diseases, promoted by the Italian Foundation of Multiple Sclerosis and endorsed by the Italian Society of Neurology will greatly augment our scientific knowledge about the relationship between CCSVI and MS.
There is the theoretical possibility that the venous drainage of autoimmune lymphocytes from the brain may cause some endothelial changes during the longstanding disease course of MS, maybe in combination with immunosuppressive therapies. Yet even if this were the case, this is insufficient to justify invasive, costly and potentially dangerous manipulations of the deep cervical venous system in MS patients.
Therefore, both the EFNS and the ENS Multiple Sclerosis Scientist Panel and ECTRIMS Executive Committee emphasize the high risk and absence of a scientific basis for “liberation procedures” in MS patients. All societies are in full accord with the Multiple Sclerosis International Federation statement on CCSVI.(http://www.msif.org/en/research/msif_on_ccsvi.html)
Literature:
Allen IV. (1981) The pathology of multiple sclerosis fact, fiction and hypothesis. Neuropathol Appl Neurobiol;7: 169
Baracchini C, Perini P, Calabrese M, Causin F, Rinaldi F, Gallo P (2011): No evidence of Chronic cerebrospinal venous insufficiency at Multiple Sclerosis onset. Ann Neurol 69:90-99.
Compston A and Coles A (2008): Multiple Sclerosis. Lancet 372:1502-1517.
Doepp F, Paul F, Valdueza JM, Schmierer K, Schreiber SJ (2010): No cerebrocervical venous congestion in patients with multiple sclerosis. Ann Neurol 68:173-183.
Gius JA and Grier DH (1950): Venous adaptation following bilateral radical neck dissection with excision of the jugular veins. Surgery 28:305-321.
Krogias C, Schroeder A, Wiendl H, Hohlfeld R, Gold R (2010): Chronic cerebrospinal venous insufficiency and multiple sclerosis: critical analysis and first observation in an unselected cohort of MS patients. Nervenarzt, 81:740-746.
Lucchinetti C, Bruck W et al. (2000): Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination. Ann Neurol 47:707-717.
Mayer CA, Pfeilschifter W, Lorenz MW, Nedelmann M, Bechmann I, Steinmetz H, Ziemann U (2011): The perfect crime? CCSVI not leaving a trace in MS. J Neurol Neurosurg Psychiatry (2011) doi:10.1136/jnnp.2010.231613.
Nedelmann M, Kaps M, Mueller-Forell W (2009): Venous obstruction and jugular valve insufficiency in diopathic intracranial hypertension. J Neurol 256:964-969.
Schreiber SJ, Doepp F, Klingbeil R, et al. (2005): Internal jugular vein valve incompetence and intracranial venous anatomy in transient global amnesia. J Neurol Neurosurg Psychiatry 76:509-513.
Zamboni P (2006): The big idea: iron-dependent inflammation in venous disease and proposed parallels in multiple sclerosis. J R Soc Med. 99:589-93.
Zamboni P, Galeotti R, Menegatti E, et al. (2009a): Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J Neurol Neurosurg Psychiatry 80:392-399.
Zamboni P, Galeotti R, Menegatti E, et al. (2009b): A prospective open-label study of endovascular treatment of chronic cerebrospinal venous insufficiency. J Vasc Surg 50:1348-1358.
Zivadinov R, Marr K, Ramanathan M, et al. (2010): Combined transcranial and extracranial venous Doppler evaluation (CTEVD Study). Description and the interim results of an epidemiological study of the prevalence of chronic cerebrospinal venous insufficiency in MS and related diseases. Neurology 74(suppl. 2):A545 [P06.144]
Comment by Gian Luigi Lenzi
In Italy, many important newspapers are publishing adverts asking for support to this new scientific and therapeutic discovery by Zamboni that “may halt or improve symptoms due to MS“. The support may be given through sending an SMS, which means giving one or two Euros. The advert shows a nice female head restrained like the cork of a bottle by iron wires.
Neuropenews is asking a comment from the firmataries of the above-shown article.





9 comments
Dear Prof Lenzi and Friends,
The Zamboni-derived protocols have other variables included.
Take into account the peri and post procedural medications administred. The large majority of subjects undergoing venous balooning in private hospitals, at my knowledge, are treated with oral mesoglycan (PRISMA) and subcutaneous heparin (CLEXANE) for days/weeks.
The “off label” use of any drug should be adopted with an appropriate informed consent and brings an add on risk to the invasive procedure itself.
In Germany the CCSVI pressure has significantly lowered. In few of a number of NEGATIVE studies also in early MS (CIS), where no abnormalities were detected, the rationale gets less.
Ralf Gold (Chair of the EFNS Panel on Demyelinating Diseases)
Ralf Gold
(Science Program)
Dr. Gold has received personal compensation for activities with Bayer Pharmaceuticals Corporation, Biogen Idec, Merck Serono, Teva Neuroscience. Dr. Gold has received personal compensation in an editorial capacity for Therapeutic Advances in Neurological Disorders. Dr. Gold has received (royalty or license fee or contractual rights) payments from Biogen Idec. Dr. Gold has received research support from Bayer Pharmaceuticals Corporation, Biogen Idec, Merck Serono, Novartis and Teva Neuroscience.
No aggressiveness from our patients and patients’ societies about CCSVI. In our neurological practice with MS patients CCSVI is marginal, and without aggressiveness from the media. It is a “no subject at the moment.”
I have the same comments as Michel Clanet. CCSVI is a no-subject at the moment.
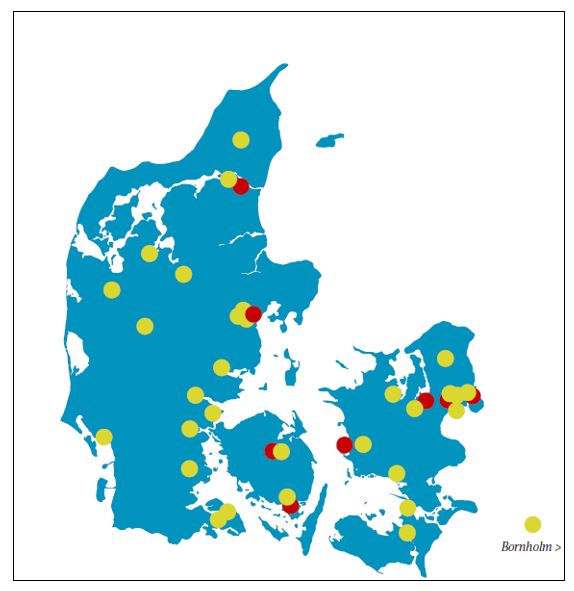
It is rather quiet regarding CCSVI. The press is taking no interest in the matter. The majority of patients appreciate the futility of the concept and only a small group is trying to maintain the pressure on media discussion. The MS Society is not supporting research in CCSVI and has not expressed any statement in support of CCSVI. They are awaiting the results of a rather small Danish study that has now been finalized in our institution. We don’t know what will happen when the results are reported.
I am writing on behalf of the Hungarian MS Advisory Board. Since strong supportive evidence has not been produced, any procedure to mechanically correct the purported CCSVI is acceptable only in a well controlled clinical trial under proper ethical permissions.
In Italy, because of the key role of Prof. P. Zamboni in promoting the theory of the pathogenetic role of CCSVI in MS and because of the abuse of the media for this topic without appropriate criticism, the public interest of the CCSVI is still very high.
We regret that the matter has moved from science to a public debate guided by fideistic approaches.
A clinical trial on MS patients treated with angioplasty is now starting in Italy with the sponsorship of the Regione Emilia Romagna coordinated by Prof. P. Zamboni. At the same time a very large multicenter epidemiologically study, sponsored by the Italian MS Society involving 2000 subjects including MS patients, patients with neurodegenerative disorders and normal controls, has been almost completed.
The object of the study is to clarify the relationship between MS and CCSVI.
I completely share the opinions expressed by the President of the Italian Society of Neurology, Prof. G. Comi. NEUROPENEWS is looking forward for the results of these trials, in the interest of the MS patients, beyond media pressure and in a scientific FORUM.