by Reinhold Schmidt
Longitudinal population-based studies have provided important information on the prevalence and incidence of dementia and it´s subtypes in the general population However, such studies consider incident dementia as an endpoint because their design is not suited to subsequently follow the natural course of cognitive and functional decline once dementia occurred. The burden of dementia on caregivers and healthcare systems in terms of cost, needs and resource utilisation is normally also outside the scope of classical cohort studies as is the mode of patient referral and diagnosis-making. As a consequence data on routine clinical practice of primary care services and specialised care on a regional basis are scarce. Prospectively designed case registries can provide such data and thus represent an important complimentary approach in dementia research. Such registries are standard for many diseases, but uncommon in the field of dementing disorders. The Austrian Alzheimer Society which is a partner Society of the Austrian Neurological Society (ÖGN) finances a prospective dementia registry (PRODEM-Austria) on a national basis on non-institutionalized dementia cases. This registry extends previous research by assessing the current diagnostic and therapeutic practice in daily routine. Besides clinical evaluation it also includes MR imaging and biobanking with 6 months follow-up over a total observational period of 2 years and will thus complement longitudinal studies on the course and prognostic determinants of different dementia types. The systematic evaluation of the use of auxiliary community services at study entry and during the disease course and the assessment of the physical, psychological and economic burden on caregivers is another important feature of this project.
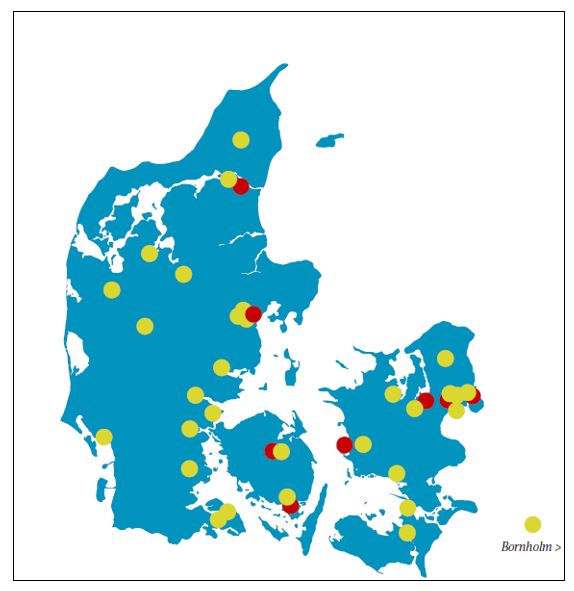
Recruiting centers include memory clinics from four University neurological and psychiatric departments and from eight district hospitals in Austria.
Investigators represent the specialties of neurology and/or psychiatry. The registry has been prospectively designed with all centers using identical protocols with examinations at baseline and every six months over an observational period of 24 months. Inclusion criteria are (1) dementia diagnosis according to DSM-IV criteria (7)], (2) non-institutionalization but no need for 24-hour care, (3) availability of a caregiver who agrees to provide information on the patients’ and his/her own condition. Patients are excluded from the study if they are unable to sign an informed consent or if co-morbidities are likely to preclude termination of the study.
At this point more than 500 dementia patients are included and the registry results provide a mirror of outpatient dementia care in Austria. With more than 80% Alzheimer’s disease is the by far most common diagnosis of patients referred to Austrian memory clinics. Vascular dementia and Lewy Body dementia (LBD) account for approximately 5% of referrals each. If a structured interview towards key symptoms of LBD is applied the frequency of both probable and possible LBD increases substantially. In such instance 5% of patients are classified as probable and 14% as possible LBD. The mean latency between onset of dementia symptoms and first visit to a memory clinic is 33 months. As can be seen from the figure it is a family member or a caregiver who initiates the referral in the prevailing portion of patients.The symptoms that lead to referral are memory complaints (79%) followed by impairment in activities of daily living (36%) and behavioral abnormalities (25%).
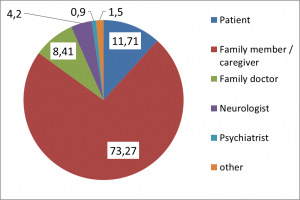
Figure 2. Persons taking the initiative to refer patients to a memory clinic. Numbers are percentages
At first visit one out of five patients has receives approved dementia drugs. Approximately 75% of patients live at home with their families, the most commonly used medical care services are general practioners which are attended on a monthly basis in almost 80% of patients, regular appointments with neurologist occur in 29% of patients. Austria has a care allowance system with an increasing amount of money given by the state based on the magnitude of disability. The range of allowance is from €154 to €1655 per month; and even though all dementia patients are eligible only 61% of patients referred to a memory clinic obtains such financial benefits.
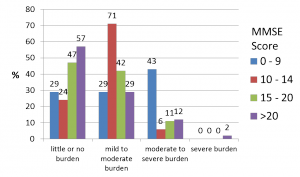
Spouses and children provide the patients care in more than 80%. And support services for carers are rarely used. Only 3% of carers visit support groups. Caregiver burden as determined by the Zarit Caregiver Burden Scale depends on the severity of dementia is high and even in patients with MMSE scores above 20 almost 43% of carers report at least mild to moderate burden.
PRODEM-Austria is an important national project as it allows to obtain important information on dementia care in Austria and there exists a link to the Ministry of Social Affairs which considers PRODEM results as an important source in planning and optimizing support systems for dementia care in Austria.
Reinhold Schmidt is Professor of Neurology and Head of the Clinical Department of Neurogeriatrics at the Medical University Graz, Austria