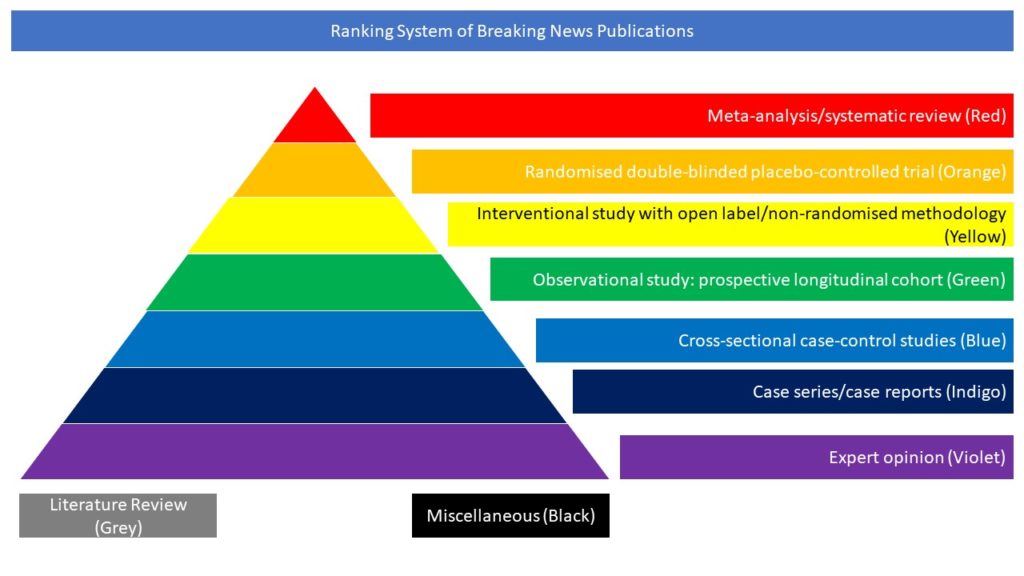
Case series/case reports (Indigo)
Read on for our highlighted selection of Covid-related case series and case reports from the scientific press for February 2022:
- The blood-brain barrier is dysregulated in COVID-19 and serves as a CNS entry route for SARS-CoV-2
- EEG changes in intensive care patients diagnosed with COVID-19: a prospective clinical study
The blood-brain barrier is dysregulated in COVID-19 and serves as a CNS entry route for SARS-CoV-2
Neurological complications are common in COVID-19. Although SARS-CoV-2 has been detected in patients’ brain tissues, its entry routes and resulting consequences are not well understood. Here, the authors show a pronounced upregulation of interferon signaling pathways of the neurovascular unit in fatal COVID-19. By investigating the susceptibility of human induced pluripotent stem cell (hiPSC)-derived brain capillary endothelial-like cells (BCECs) to SARS-CoV-2 infection, they found that BCECs were infected and recapitulated transcriptional changes detected in vivo. While BCECs were not compromised in their paracellular tightness, the authors found SARS-CoV-2 in the basolateral compartment in transwell assays after apical infection, suggesting active replication and transcellular transport of virus across the blood-brain barrier (BBB) in vitro. Moreover, entry of SARS-CoV-2 into BCECs could be reduced by anti-spike-, anti-angiotensin-converting enzyme 2 (ACE2)-, and anti-neuropilin-1 (NRP1)-specific antibodies or the transmembrane protease serine subtype 2 (TMPRSS2) inhibitor nafamostat. The authors concluded that their data provide strong support for SARS-CoV-2 brain entry across the BBB resulting in increased interferon signaling.
Krasemann S, Haferkamp U, Pfefferle S, Woo MS, Heinrich F, Schweizer M, Appelt-Menzel A, Cubukova A, Barenberg J, Leu J, Hartmann K, Thies E, Littau JL, Sepulveda-Falla D, Zhang L, Ton K, Liang Y, Matschke J, Ricklefs F, Sauvigny T, Sperhake J, Fitzek A, Gerhartl A, Brachner A, Geiger N, König EM, Bodem J, Franzenburg S, Franke A, Moese S, Müller FJ, Geisslinger G, Claussen C, Kannt A, Zaliani A, Gribbon P, Ondruschka B, Neuhaus W, Friese MA, Glatzel M, Pless O. The blood-brain barrier is dysregulated in COVID-19 and serves as a CNS entry route for SARS-CoV-2. Stem Cell Reports. 2022 Jan 3:S2213-6711(21)00650-0. doi: 10.1016/j.stemcr.2021.12.011.
EEG changes in intensive care patients diagnosed with COVID-19: a prospective clinical study
Coronavirus disease (COVID-19) is an infectious disease caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease was declared a pandemic on March 11th, 2020, by the World Health Organization (WHO). There has been a substantial increase in the epileptic seizures and status epilepticus reported in the pandemic period. In this context, the authors aimed with this study to identify the electroencephalography (EEG) features of patients admitted to the intensive care unit with the diagnosis of COVID-19 and to look for any specific patterns in these features. The material of this study primarily comprised the neurological evaluations and continuous EEG recordings of 87 intensive care patients who were diagnosed with COVID-19. In addition, demographic and clinical features and comorbid conditions of these patients were also analyzed, and any correlation thereof was investigated. The EEG data of 87 patients who were diagnosed with COVID-19 and were followed up in the intensive care unit were recorded and then analyzed. Abnormal EEG findings were detected in 93.1% (n = 81) of the patients, which were found to increase significantly with age (p < 0.001). The mean age of patients with specific epileptiform abnormalities on EEG was found to be significantly higher than those with non-specific abnormalities. Epileptiform discharges were seen in 37.9% (n = 33) of the patients. Nonconvulsive status epilepticus (NCSE) was detected in 5.7% of the patients, and antiepileptic drugs were started in 25 (28.7%) of the patients. The authors concluded that statistically significant EEG changes were observed in the continuous EEGs of the patients followed up in the intensive care unit due to COVID-19 infection. However, further studies are needed to associate the EEG changes observed in the COVID-19 patients with the epileptogenesis of COVID-19 infection.
Karadas O, Ozturk B, Sonkaya AR, Duzgun U, Shafiyev J, Eskin MB, Bostan T, Ozon AO. EEG changes in intensive care patients diagnosed with COVID-19: a prospective clinical study. Neurol Sci. 2022 Jan 23. doi: 10.1007/s10072-021-05818-7.