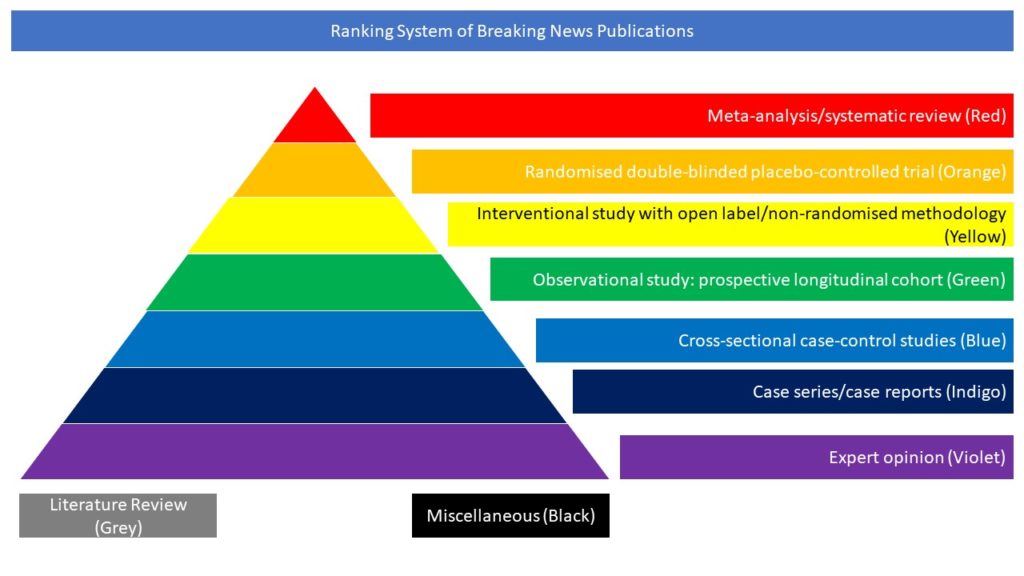
Cross-sectional case-control studies (Blue)
Read on for the first half of our highlighted selection of Covid-related cross-sectional case control studies from the scientific press for January 2022:
- BNT162b2 Vaccine Booster and Mortality Due to COVID-19
- Protection against COVID-19 by BNT162b2 Booster across Age Groups
- Two-dose ChAdOx1 nCoV-19 vaccine protection against COVID-19 hospital admissions and deaths over time: a retrospective, population-based cohort study in Scotland and Brazil
- Heterologous ChAdOx1 nCoV-19 and BNT162b2 prime-boost vaccination elicits potent neutralizing antibody responses and T cell reactivity against prevalent SARS-CoV-2 variants
- Risk of venous thrombotic events and thrombocytopenia in sequential time periods after ChAdOx1 and BNT162b2 COVID-19 vaccines: A national cohort study in England
- Disentangling post-vaccination symptoms from early COVID-19
- Severity of Illness in Persons Infected With the SARS-CoV-2 Delta Variant vs Beta Variant in Qatar
- Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization
- Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2
- Report 49: Growth, population distribution and immune escape of Omicron in England
- Effectiveness of mRNA-1273 against delta, mu, and other emerging variants of SARS-CoV-2: test negative case-control study
BNT162b2 Vaccine Booster and Mortality Due to COVID-19
The emergence of the B.1.617.2 (delta) variant of severe acute respiratory syndrome coronavirus 2 and the reduced effectiveness over time of the BNT162b2 vaccine (Pfizer–BioNTech) led to a resurgence of coronavirus disease 2019 (COVID-19) cases in populations that had been vaccinated early. On July 30, 2021, the Israeli Ministry of Health approved the use of a third dose of BNT162b2 (booster) to cope with this resurgence. Evidence regarding the effectiveness of the booster in lowering mortality due to COVID-19 is still needed. In this article the authors obtained data for all members of Clalit Health Services who were 50 years of age or older at the start of the study and had received two doses of BNT162b2 at least 5 months earlier. The mortality due to COVID-19 among participants who received the booster during the study period (booster group) was compared with that among participants who did not receive the booster (nonbooster group). A Cox proportional-hazards regression model with time-dependent covariates was used to estimate the association of booster status with death due to COVID-19, with adjustment for sociodemographic factors and coexisting conditions. A total of 843,208 participants met the eligibility criteria, of whom 758,118 (90%) received the booster during the 54-day study period. Death due to COVID-19 occurred in 65 participants in the booster group (0.16 per 100,000 persons per day) and in 137 participants in the nonbooster group (2.98 per 100,000 persons per day). The adjusted hazard ratio for death due to COVID-19 in the booster group, as compared with the nonbooster group, was 0.10 (95% confidence interval, 0.07 to 0.14; P<0.001). The authors concluded highlighting that participants who received a booster at least 5 months after a second dose of BNT162b2 had 90% lower mortality due to COVID-19 than participants who did not receive a booster.
Arbel R, Hammerman A, Sergienko R, Friger M, Peretz A, Netzer D, Yaron S. BNT162b2 Vaccine Booster and Mortality Due to COVID-19. N Engl J Med. 2021 Dec 23;385(26):2413-2420. doi: 10.1056/NEJMoa2115624.
Protection against COVID-19 by BNT162b2 Booster across Age Groups
After promising initial results from the administration of a third (booster) dose of the BNT162b2 messenger RNA vaccine (Pfizer–BioNTech) to persons 60 years of age or older, the booster campaign in Israel was gradually expanded to persons in younger age groups who had received a second dose at least 5 months earlier. In this article the authors extracted data for the period from July 30 to October 10, 2021, from the Israel Ministry of Health database regarding 4,696,865 persons 16 years of age or older who had received two doses of BNT162b2 at least 5 months earlier. In the primary analysis, they compared the rates of confirmed coronavirus disease 2019 (COVID-19), severe illness, and death among those who had received a booster dose at least 12 days earlier (booster group) with the rates among those who had not received a booster (nonbooster group). In a secondary analysis, they compared the rates in the booster group with the rates among those who had received a booster 3 to 7 days earlier (early postbooster group). Poisson regression models were used to estimate rate ratios after adjusting for possible confounding factors. The rate of confirmed infection was lower in the booster group than in the nonbooster group by a factor of approximately 10 (range across five age groups, 9.0 to 17.2) and was lower in the booster group than in the early postbooster group by a factor of 4.9 to 10.8. The adjusted rate difference ranged from 57.0 to 89.5 infections per 100,000 person-days in the primary analysis and from 34.4 to 38.3 in the secondary analysis. The rates of severe illness in the primary and secondary analyses were lower in the booster group by a factor of 17.9 (95% confidence interval [CI], 15.1 to 21.2) and 6.5 (95% CI, 5.1 to 8.2), respectively, among those 60 years of age or older and by a factor of 21.7 (95% CI, 10.6 to 44.2) and 3.7 (95% CI, 1.3 to 10.2) among those 40 to 59 years of age. The adjusted rate difference in the primary and secondary analyses was 5.4 and 1.9 cases of severe illness per 100,000 person-days among those 60 years of age or older and 0.6 and 0.1 among those 40 to 59 years of age. Among those 60 years of age or older, mortality was lower by a factor of 14.7 (95% CI, 10.0 to 21.4) in the primary analysis and 4.9 (95% CI, 3.1 to 7.9) in the secondary analysis. The adjusted rate difference in the primary and secondary analyses was 2.1 and 0.8 deaths per 100,000 person-days. The authors concluded that across the age groups studied, rates of confirmed COVID-19 and severe illness were substantially lower among participants who received a booster dose of the BNT162b2 vaccine than among those who did not.
Bar-On YM, Goldberg Y, Mandel M, Bodenheimer O, Freedman L, Alroy-Preis S, Ash N, Huppert A, Milo R. Protection against COVID-19 by BNT162b2 Booster across Age Groups. N Engl J Med. 2021 Dec 23;385(26):2421-2430. doi: 10.1056/NEJMoa2115926.
Two-dose ChAdOx1 nCoV-19 vaccine protection against COVID-19 hospital admissions and deaths over time: a retrospective, population-based cohort study in Scotland and Brazil
Reports suggest that COVID-19 vaccine effectiveness is decreasing, but whether this reflects waning or new SARS-CoV-2 variants—especially delta (B.1.617.2)—is unclear. In this study the authors investigated the association between time since two doses of ChAdOx1 nCoV-19 vaccine and risk of severe COVID-19 outcomes in Scotland (where delta was dominant), with comparative analyses in Brazil (where delta was uncommon). In this retrospective, population-based cohort study in Brazil and Scotland, the authors linked national databases from the EAVE II study in Scotland; and the COVID-19 Vaccination Campaign, Acute Respiratory Infection Suspected Cases, and Severe Acute Respiratory Infection/Illness datasets in Brazil for vaccination, laboratory testing, clinical, and mortality data. They defined cohorts of adults (aged ≥18 years) who received two doses of ChAdOx1 nCoV-19 and compared rates of severe COVID-19 outcomes (ie, COVID-19 hospital admission or death) across fortnightly periods, relative to 2–3 weeks after the second dose. Entry to the Scotland cohort started from May 19, 2021, and entry to the Brazil cohort started from Jan 18, 2021. Follow-up in both cohorts was until Oct 25, 2021. Poisson regression was used to estimate rate ratios (RRs) and vaccine effectiveness, with 95% CIs. 1 972 454 adults received two doses of ChAdOx1 nCoV-19 in Scotland and 42 558 839 in Brazil, with longer follow-up in Scotland because two-dose vaccination began earlier in Scotland than in Brazil. In Scotland, RRs for severe COVID-19 increased to 2·01 (95% CI 1·54–2·62) at 10–11 weeks, 3·01 (2·26–3·99) at 14–15 weeks, and 5·43 (4·00–7·38) at 18–19 weeks after the second dose. The pattern of results was similar in Brazil, with RRs of 2·29 (2·01–2·61) at 10–11 weeks, 3·10 (2·63–3·64) at 14–15 weeks, and 4·71 (3·83–5·78) at 18–19 weeks after the second dose. In Scotland, vaccine effectiveness decreased from 83·7% (95% CI 79·7–87·0) at 2–3 weeks, to 75·9% (72·9–78·6) at 14–15 weeks, and 63·7% (59·6–67·4) at 18–19 weeks after the second dose. In Brazil, vaccine effectiveness decreased from 86·4% (85·4–87·3) at 2–3 weeks, to 59·7% (54·6–64·2) at 14–15 weeks, and 42·2% (32·4–50·6) at 18–19 weeks. The authors concluded that they found waning vaccine protection of ChAdOx1 nCoV-19 against COVID-19 hospital admissions and deaths in both Scotland and Brazil, this becoming evident within three months of the second vaccine dose. They underlined that consideration needs to be given to providing booster vaccine doses for people who have received ChAdOx1 nCoV-19.
Katikireddi SV, Cerqueira-Silva T, Vasileiou E, Robertson C, Amele S, Pan J, Taylor B, Boaventura V, Werneck GL, Flores-Ortiz R, Agrawal U, Docherty AB, McCowan C, McMenamin J, Moore E, Ritchie LD, Rudan I, Shah SA, Shi T, Simpson CR, Barreto ML, Oliveira VA, Barral-Netto M, Sheikh A. Two-dose ChAdOx1 nCoV-19 vaccine protection against COVID-19 hospital admissions and deaths over time: a retrospective, population-based cohort study in Scotland and Brazil. Lancet. 2021 Dec 20:S0140-6736(21)02754-9. doi: 10.1016/S0140-6736(21)02754-9.
Heterologous ChAdOx1 nCoV-19 and BNT162b2 prime-boost vaccination elicits potent neutralizing antibody responses and T cell reactivity against prevalent SARS-CoV-2 variants
Heterologous COVID-19 vaccination regimens combining vector- and mRNA-based vaccines are already administered, but data on solicited adverse reactions, immunological responses and elicited protection are limited. The objective of this study was to evaluate the reactogenicity and humoral as well as cellular immune responses towards most prevalent SARS-CoV-2 variants after a heterologous ChAdOx1 nCoV-19 BNT162b2 prime-boost vaccination. The authors analysed a cohort of 26 clinic employees aged 25-46 (median 30.5) years who received a ChAdOx1 nCoV-19 prime followed by a BNT162b2 boost after an 8-week interval. Serological data were compared to a cohort which received homologous BNT162b2 vaccination with a 3-week interval (14 individuals aged 25-65, median 42). Self-reported solicited symptoms after ChAdOx1 nCoV-19 prime were in line with previous reports and more severe than after the BNT162b2 boost. Antibody titres increased significantly over time resulting in strong neutralization titres two weeks after the BNT162b2 boost and subsequently slightly decreased over the course of 17 weeks. At the latest time point measured, all analysed sera retained neutralizing activity against the currently dominant Delta (B.1.617.2) variant. Two weeks post boost, neutralizing activity against the Alpha (B.1.1.7) and immune-evading Beta (B.1.351) variant was ∼4-fold higher than in individuals receiving homologous BNT162b2 vaccination. No difference was observed in neutralization of Kappa (B.1.617.1). In addition, heterologous vaccination induced CD4+ and CD8+ T cells reactive to SARS-CoV-2 spike peptides of all analysed variants; Wuhan-Hu-1, Alpha, Beta, Gamma (P.1), and Delta. In conclusion, heterologous ChAdOx1 nCoV-19 / BNT162b2 prime-boost vaccination is not associated with serious adverse events and induces potent humoral and cellular immune responses. The Alpha, Beta, Delta, and Kappa variants of spike are potently neutralized by sera from all participants and reactive T cells recognize spike peptides of all tested variants. These results suggest that this heterologous vaccination regimen is at least as immunogenic and protective as homologous vaccinations and also offers protection against current variants of concern.
Groß R, Zanoni M, Seidel A, Conzelmann C, Gilg A, Krnavek D, Erdemci-Evin S, Mayer B, Hoffmann M, Pöhlmann S, Liu W, Hahn BH, Beil A, Kroschel J, Jahrsdörfer B, Schrezenmeier H, Kirchhoff F, Münch J, Müller JA. Heterologous ChAdOx1 nCoV-19 and BNT162b2 prime-boost vaccination elicits potent neutralizing antibody responses and T cell reactivity against prevalent SARS-CoV-2 variants. EBioMedicine. 2021 Dec 17;75:103761. doi: 10.1016/j.ebiom.2021.103761.
Risk of venous thrombotic events and thrombocytopenia in sequential time periods after ChAdOx1 and BNT162b2 COVID-19 vaccines: A national cohort study in England
Thrombosis with thrombocytopenia, or thrombocytopenia on its own, have been reported after COVID-19 vaccines. In this article the authors assessed the risk after ChAdOx1 adenovirus-vector and BNT162b2 mRNA vaccines in a national cohort study in England. Hospital admissions for a cerebral venous thrombosis (CVT), other venous thrombosis or thrombocytopenia between 30th November 2020 and 18th April 2021 were linked to the national COVID-19 immunisation register. The incidence of events by dose in pre-defined post-vaccination risk periods relative to the unvaccinated cohort was estimated after adjustment for age, gender, co-morbidities, care home residency and health/social care worker status. Elevated relative incidence (RI) estimates with p<0.001 were considered strong evidence of an association. The RI for CVT after a first ChAdOx1 dose in 15-39 and 40-64 year olds was 8.7 (95% confidence interval 5.8-13.0) and 2.2 (1.4-3.2) respectively, p<0.001. The elevated risk period in 15-39 year olds was highest 4-13 days post-vaccination (16.3, 9.9-27.0). The attributable risk (AR) was 16.1 per million doses for 15-39 and 3.2 per million for 40-64 year olds. RIs for other thrombosis admissions were elevated in these age groups with ARs of 36.3 and 16.4 per million respectively as were RIs for thrombocytopenia, with ARs of 11.3 and 10.1 per million respectively. No elevated RIs were found for 65+ year olds or after a second ChAdOx1 dose, nor for BNT162b2 vaccine recipients of any age. This epidemiological study shows an increased risk of thrombotic episodes and thrombocytopenia in adults under 65 years of age within a month of a first dose of ChAdOx1 vaccine but not after the BNT162b2 vaccine.
Andrews NJ, Stowe J, Ramsay ME, Miller E. Risk of venous thrombotic events and thrombocytopenia in sequential time periods after ChAdOx1 and BNT162b2 COVID-19 vaccines: A national cohort study in England. Lancet Reg Health Eur. 2022 Feb;13:100260. doi: 10.1016/j.lanepe.2021.100260.
Disentangling post-vaccination symptoms from early COVID-19
Identifying and testing individuals likely to have SARS-CoV-2 is critical for infection control, including post-vaccination. Vaccination is a major public health strategy to reduce SARS-CoV-2 infection globally. Some individuals experience systemic symptoms post-vaccination, which overlap with COVID-19 symptoms. This study compared early post-vaccination symptoms in individuals who subsequently tested positive or negative for SARS-CoV-2, using data from the COVID Symptom Study (CSS) app. The authors conducted a prospective observational study in 1,072,313 UK CSS participants who were asymptomatic when vaccinated with Pfizer-BioNTech mRNA vaccine (BNT162b2) or Oxford-AstraZeneca adenovirus-vectored vaccine (ChAdOx1 nCoV-19) between 8 December 2020 and 17 May 2021, who subsequently reported symptoms within seven days (N=362,770) (other than local symptoms at injection site) and were tested for SARS-CoV-2 (N=14,842), aiming to differentiate vaccination side-effects per se from superimposed SARS-CoV-2 infection. The post-vaccination symptoms and SARS-CoV-2 test results were contemporaneously logged by participants. Demographic and clinical information (including comorbidities) were recorded. Symptom profiles in individuals testing positive were compared with a 1:1 matched population testing negative, including using machine learning and multiple models considering UK testing criteria.
Differentiating post-vaccination side-effects alone from early COVID-19 was challenging, with a sensitivity in identification of individuals testing positive of 0.6 at best. Most of these individuals did not have fever, persistent cough, or anosmia/dysosmia, requisite symptoms for accessing UK testing; and many only had systemic symptoms commonly seen post-vaccination in individuals negative for SARS-CoV-2 (headache, myalgia, and fatigue). The authors concluded that post-vaccination symptoms per se cannot be differentiated from COVID-19 with clinical robustness, either using symptom profiles or machine-derived models. Individuals presenting with systemic symptoms post-vaccination should be tested for SARS-CoV-2 or quarantining, to prevent community spread.
Canas LS, Österdahl MF, Deng J, Hu C, Selvachandran S, Polidori L, May A, Molteni E, Murray B, Chen L, Kerfoot E, Klaser K, Antonelli M, Hammers A, Spector T, Ourselin S, Steves C, Sudre CH, Modat M, Duncan EL. Disentangling post-vaccination symptoms from early COVID-19. EClinicalMedicine. 2021 Dec;42:101212. doi: 10.1016/j.eclinm.2021.101212.
Severity of Illness in Persons Infected With the SARS-CoV-2 Delta Variant vs Beta Variant in Qatar
The Delta variant is now the predominant circulating SARS-CoV-2 strain worldwide. Severity of illness in persons infected with the SARS-CoV-2 Delta variant compared with the Beta variant is not known. The objective of this study was to directly compare clinical outcomes in persons infected with the SARS-CoV-2 Delta variant vs those infected with the Beta variant in Qatar. This retrospective cohort study used data from the national COVID-19 database in Qatar, which includes information on all individuals who were ever tested for SARS-CoV-2 using a reverse transcriptase–polymerase chain reaction test and all individuals who received any SARS-CoV-2 vaccine in Qatar. Among persons with confirmed SARS-CoV-2 infection between March 22 and July 7, 2021, those infected with the Delta variant were identified and were propensity score matched with control individuals infected with the Beta variant. The variants were ascertained by variant genotyping of the positive samples. The main outcomes were admission to the hospital, admission to the intensive care unit, use of supplemental oxygen, use of high-flow oxygen, receipt of mechanical ventilation, or death among those infected with the Delta or Beta variant overall and stratified by vaccination status. Among 1427 persons infected with the Delta variant (252 [55.9%] male; median age, 34 years [IQR, 17-43 years]) and 5353 persons infected with the Beta variant (233 [51.7%] male; median age, 34 years [IQR, 17-45 years]), 451 propensity score–matched pairs were identified. Persons infected with the Delta variant were more likely to be hospitalized (27.3% [95% CI, 23.2%-31.6%] vs 20.0% [95% CI, 16.4-24.0]; P = .01) or to have mild-moderate or severe-critical disease outcomes (27.9% [95% CI, 23.8%-32.3%] vs 20.2% [95% CI, 16.6%-24.2%]; P = .01) compared with persons infected with the Beta variant. Infection with the Delta variant was independently associated with higher odds of experiencing any adverse outcome (adjusted odds ratio [aOR], 2.53; 95% CI, 1.72-3.72). Compared with being unvaccinated, being vaccinated with a second dose more than 3 months before infection was associated with lower odds of any adverse outcome among persons infected with the Delta variant (aOR, 0.11; 95% CI, 0.04-0.26) and among those infected with the Beta variant (aOR, 0.22; 95% CI, 0.05-0.98). Protection was similar among those who received a second vaccine dose less than 3 months before infection, but having received only a single dose was not associated with a lower odds of any severe outcome among those infected with the Delta variant (aOR, 1.12; 95% CI, 0.41-3.06) or those infected with the Beta variant (aOR, 0.74; 95% CI, 0.20-2.72). In this cohort study of persons with COVID-19 in Qatar, infection with the SARS-CoV-2 Delta variant was associated with more severe disease than was infection with the Beta variant. Being unvaccinated was associated with greater odds of severe-critical disease.
Butt AA, Dargham SR, Chemaitelly H, Al Khal A, Tang P, Hasan MR, Coyle PV, Thomas AG, Borham AM, Concepcion EG, Kaleeckal AH, Latif AN, Bertollini R, Abou-Samra AB, Abu-Raddad LJ. Severity of Illness in Persons Infected With the SARS-CoV-2 Delta Variant vs Beta Variant in Qatar. JAMA Intern Med. 2021 Dec 22. doi: 10.1001/jamainternmed.2021.7949.
Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization
The emergence of Omicron (Pango lineage B.1.1.529), first identified in Botswana and South Africa, may compromise vaccine effectiveness and lead to re-infections. In this study the authors investigated whether Omicron escapes antibody neutralization in South Africans vaccinated with Pfizer BNT162b2. They also investigated if Omicron requires the ACE2 receptor to infect cells. Confirmed live Omicron virus from an infected person in South Africa was isolated and sequence and compared plasma neutralization of Omicron relative to an ancestral SARS-CoV-2 strain, observing that Omicron still required ACE2 to infect. For neutralization, blood samples were taken soon after vaccination from participants who were vaccinated and previously infected or vaccinated with no evidence of previous infection. Neutralization of ancestral virus was much higher in infected and vaccinated versus vaccinated only participants but both groups showed a 22-fold escape from vaccine elicited neutralization by the Omicron variant. However, in the previously infected and vaccinated group, the level of residual neutralization of Omicron was similar to the level of neutralization of ancestral virus observed in the vaccination only group. These data support the notion that, provided high neutralization capacity is elicited by vaccination/boosting approaches, reasonable effectiveness against Omicron may be maintained.
Sandile Cele , Laurelle Jackson , David S. Khoury , Khadija Khan , Thandeka Moyo-Gwete , Houriiyah Tegally , James Emmanuel San , Deborah Cromer , Cathrine Scheepers , Daniel Amoako , Farina Karim , Mallory Bernstein , Gila Lustig , Derseree Archary , Muneerah Smith , Yashica Ganga , Zesuliwe Jule , Kajal Reedoy , Shi-Hsia Hwa , Jennifer Giandhari , Jonathan M. Blackburn , Bernadett I. Gosnell , Salim S. Abdool Karim , Willem Hanekom , Network for Genomic Surveillance in South Africa , COMMIT-KZN Team , Anne von Gottberg , Jinal Bhiman , Richard J. Lessells , Mahomed-Yunus S. Moosa , Miles P. Davenport , Tulio de Oliveira , Penny L. Moore & Alex Siga. Omicron extensively but incompletely escapes Pfizer BNT162b2 neutralization. Nature. doi: https://doi.org/10.1038/d41586-021-03824-5.
Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2
The Omicron (B.1.1.529) variant of SARS-CoV-2 (severe acute respiratory syndrome coronavirus) was only recently detected in southern Africa, but its subsequent spread has been extensive, both regionally and globally. It is expected to become dominant in the coming weeks, probably due to enhanced transmissibility. A striking feature of this variant is the large number of spike mutations that pose a threat to the efficacy of current COVID-19 (coronavirus disease 2019) vaccines and antibody therapies. This concern is amplified by the findings from this study. Indeed the authors found B.1.1.529 to be markedly resistant to neutralization by serum not only from convalescent patients, but also from individuals vaccinated with one of the four widely used COVID-19 vaccines. Even serum from persons vaccinated and boosted with mRNA-based vaccines exhibited substantially diminished neutralizing activity against B.1.1.529. By evaluating a panel of monoclonal antibodies to all known epitope clusters on the spike protein, the authors noted that the activity of 17 of the 19 antibodies tested were either abolished or impaired, including ones currently authorized or approved for use in patients. In addition, the authors also identified four new spike mutations (S371L, N440K, G446S, and Q493R) that confer greater antibody resistance to B.1.1.529. They concluded that the Omicron variant presents a serious threat to many existing COVID-19 vaccines and therapies, compelling the development of new interventions that anticipate the evolutionary trajectory of SARS-CoV-2.
Lihong Liu , Sho Iketani , Yicheng Guo , Jasper F-W. Chan , Maple Wang , Liyuan Liu , Yang Luo , Hin Chu , Yiming Huang , Manoj S. Nair , Jian Yu , Kenn K-H. Chik , Terrence T-T. Yuen , Chaemin Yoon , Kelvin K-W. To , Honglin Chen , Michael T. Yin , Magdalena E. Sobieszczyk , Yaoxing Huang, Harris H. Wang , Zizhang Sheng , Kwok-Yung Yuen, David D. Ho. Striking Antibody Evasion Manifested by the Omicron Variant of SARS-CoV-2. Nature. doi: https://doi.org/10.1038/d41586-021-03826-3.
Report 49: Growth, population distribution and immune escape of Omicron in England
To estimate the growth of the Omicron variant of concern and its immune escape characteristics, the authors analysed data from all PCR-confirmed SARS-CoV-2 cases in England excluding those
with a history of recent international travel. They undertook separate analyses according to two cases
definitions. For the first definition, they included all cases with a definitive negative S-gene Target
Failure (SGTF) result and specimen dates between 29/11/2021 and 11/12/2021 inclusive. For the
second definition, they included cases with a positive genotype result and specimen date between
23/11/2021 and 11/12/2021 inclusive. They chose a later start date for the SGTF definition to ensure
greater specificity of SGTF for Omicron. Logistic and Poisson regression were applied to identify factors associated with testing positive for Omicron compared to non-Omicron (mostly Delta) cases. The following predictors were explored: day, region, symptomatic status, sex, ethnicity, age band and vaccination status. The results suggest rapid growth of the frequency of the Omicron variant relative to Delta, with the exponential growth rate of its frequency estimated to be 0.34/day (95% CI: 0.33-0.35) [2.0 day doubling time] over the study period from both SGTF and genotype data. The distribution of Omicron by age, region and ethnicity currently differs markedly from Delta, with 18–29-year-olds, residents in the London region, and those of African ethnicity having significantly higher rates of infection with Omicron relative to Delta. Hospitalisation and asymptomatic infection indicators were not significantly associated with Omicron infection, suggesting at most limited changes in severity compared with Delta. To estimate the impact of Omicron on vaccine effectiveness (VE) for symptomatic infection a conditional Poisson regression was used to estimate the hazard ratio of being an Omicron case (using SGTF definition) compared with Delta, restricting the analysis to symptomatic cases and matching by day, region, 10-year age band, sex and ethnicity. A significant increased risk of an Omicron case compared to Delta was found for those with vaccine status AZ 2+weeks post-dose 2 (PD2) , Pfizer 2+w PD2, AZ 2+w post-dose 3 (PD3) and PF 2+w PD3 vaccine states with hazard ratios of 1.86 (95%CI: 1.67-2.08), 2.68 (95%CI: 2.54-2.83), 4.32 (95%CI: 3.84-4.85) and 4.07 (95%CI: 3.66-4.51), respectively, where PD3 states are categorised by the dose 1/2 vaccine used. Depending on the Delta VE estimates used, these estimates translate into Omicron VE estimates of between 0% and 20% PD2 and between 55% and 80% PD3 against Omicron, consistent with other estimates. Similar estimates were obtained using genotype data, albeit with greater uncertainty. To assess the impact of Omicron on reinfection rates the authors relied on genotype data, since SGTF is associated with a higher observed rate of reinfection, likely due to reinfections typically having higher Ct values than primary infections and therefore being subject to a higher rate of random PCR target failure. Controlling for vaccine status, age, sex, ethnicity, asymptomatic status, region and specimen
date and using conditional Poisson regression to predict reinfection status, Omicron was associated
with a 5.41 (95% CI: 4.87-6.00) fold higher risk of reinfection compared with Delta. This suggests
relatively low remaining levels of immunity from prior infection.
Neil Ferguson, Azra Ghani, Anne Cori et al. Growth, population distribution and immune escape of the Omicron in England. Imperial College London (16-12-2021), doi: https://doi.org/10.25561/93038.
Effectiveness of mRNA-1273 against delta, mu, and other emerging variants of SARS-CoV-2: test negative case-control study
The objective of this test negative case-control study was to evaluate the effectiveness of the mRNA-1273 vaccine against SARS-CoV-2 variants and assess its effectiveness against the delta variant by time since vaccination. Adult Kaiser Permanente Southern California (KPSC) members with a SARS-CoV-2 positive test sent for whole genome sequencing or a negative test from 1 March 2021 to 27 July 2021were included. Patients were divided in two groups based on two dose or one dose vaccination with mRNA-1273 (Moderna COVID-19 vaccine) ≥14 days before specimen collection versus no COVID-19 vaccination. Outcomes included infection with SARS-CoV-2 and hospital admission with COVID-19. In pre-specified analyses for each variant type, test positive cases were matched 1:5 to test negative controls on age, sex, race/ethnicity, and specimen collection date. Conditional logistic regression was used to compare odds of vaccination among cases versus controls, with adjustment for confounders. Vaccine effectiveness was calculated as (1–odds ratio)×100%. The study included 8153 cases and their matched controls. Two dose vaccine effectiveness was 86.7% (95% confidence interval 84.3% to 88.7%) against infection with the delta variant, 98.4% (96.9% to 99.1%) against alpha, 90.4% (73.9% to 96.5%) against mu, 96-98% against other identified variants, and 79.9% (76.9% to 82.5%) against unidentified variants (that is, specimens that failed sequencing). Vaccine effectiveness against hospital admission with the delta variant was 97.5% (92.7% to 99.2%). Vaccine effectiveness against infection with the delta variant declined from 94.1% (90.5% to 96.3%) 14-60 days after vaccination to 80.0% (70.2% to 86.6%) 151-180 days after vaccination. Waning was less pronounced for non-delta variants. Vaccine effectiveness against delta infection was lower among people aged ≥65 years (75.2%, 59.6% to 84.8%) than those aged 18-64 years (87.9%, 85.5% to 89.9%). One dose vaccine effectiveness was 77.0% (60.7% to 86.5%) against infection with delta. The authors concluded that two doses of mRNA-1273 were highly effective against all SARS-CoV-2 variants, especially against hospital admission with COVID-19. However, vaccine effectiveness against infection with the delta variant moderately declined with increasing time since vaccination.
Bruxvoort K J, Sy L S, Qian L, Ackerson B K, Luo Y, Lee G S et al. Effectiveness of mRNA-1273 against delta, mu, and other emerging variants of SARS-CoV-2: test negative case-control study BMJ 2021; 375 :e068848 doi:10.1136/bmj-2021-068848.