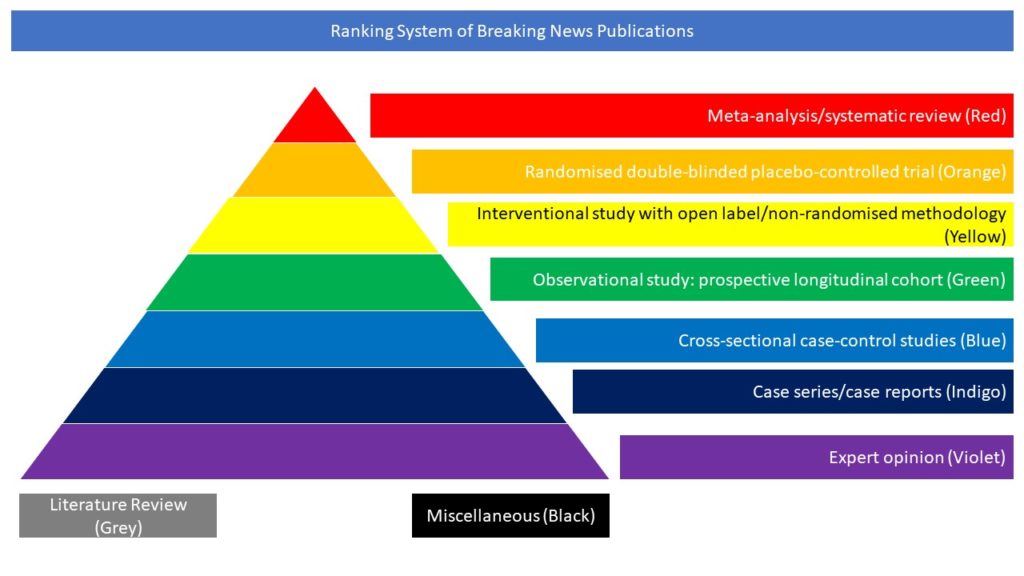
Case series/case reports (Indigo)
Autoimmune encephalitis (AE) cases post-SARS-CoV-2 infection have been reported, but the frequency is unknown. In this article the authors aimed to determine the frequency and diagnostic features of COVID-19 related AE. Residual sera from 556 consecutive Mayo Clinic Rochester patients (laboratory cohort) who underwent autoimmune encephalopathy neural IgG evaluation were tested for total antibodies against the SARS-CoV-2 spike glycoprotein using an FDA-authorized chemiluminescence assay (October 2019-December 2020). Clinical records from patients with a positive SARS-CoV-2 antibody result and available research consent were reviewed. This laboratory cohort was cross-referenced with the Department of Neurology’s COVID-related consultative experience (encephalopathy cohort, n=31). Eighteen of the laboratory cohort (3%) were SARS-CoV-2 antibody positive (April-December 2020). Diagnoses were: AE, 2; post-acute sequelae of SARS CoV-2 infection [PASC], 3; toxic-metabolic encephalopathy during COVID-19 pneumonia, 2; diverse non-COVID-19 relatable neurological diagnoses, 9; unavailable, 2. Five of the encephalopathy cohort had AE (16%, including the 2 laboratory cohort cases which overlapped) representing 0.05% of 10,384 patients diagnosed and cared for with any COVID-19 illness at Mayo Clinic Rochester in 2020. The 5 patients met definite (n=1), probable (n=1), or possible (n=3) AE diagnostic criteria; median symptom onset age was 61 years (range, 46-63), 3 were women. All 5 were neural IgG negative and 4 tested were SARS-CoV-2 PCR/IgG index negative in CSF. Phenotypes (and accompanying MRI and EEG findings) were diverse (delirium [n=5], seizures [n=2], rhombencephalitis [n=1], aphasia [n=1], and ataxia [n=1]). No ADEM cases were encountered. The 3 patients with possible AE had spontaneously resolving syndromes. One with definite limbic encephalitis was immune therapy responsive but had residual mood and memory problems. One patient with probable autoimmune rhombencephalitis died despite immune therapy. The remaining 26 encephalopathy cohort patients had toxic-metabolic diagnoses. The authors concluded that they encountered occasional cases of AE in our 2020 COVID-19 experience. Consistent with sporadic reports and small case series during the COVID-19 pandemic, and prior experience of postinfectious AE, their cases had diverse clinical presentations and were neural IgG and CSF viral particle negative. Moreover, application of diagnostic criteria assists in differentiation of AE from toxic-metabolic causes arising in the setting of systemic infection.
Sanchez CV, Theel E, Binnicker M, Toledano M, McKeon A. Autoimmune Encephalitis Post-SARS-CoV-2 Infection: Case Frequency, Findings, and Outcomes. Neurology. 2021 Oct 11:10.1212/WNL.0000000000012931. doi: 10.1212/WNL.0000000000012931.