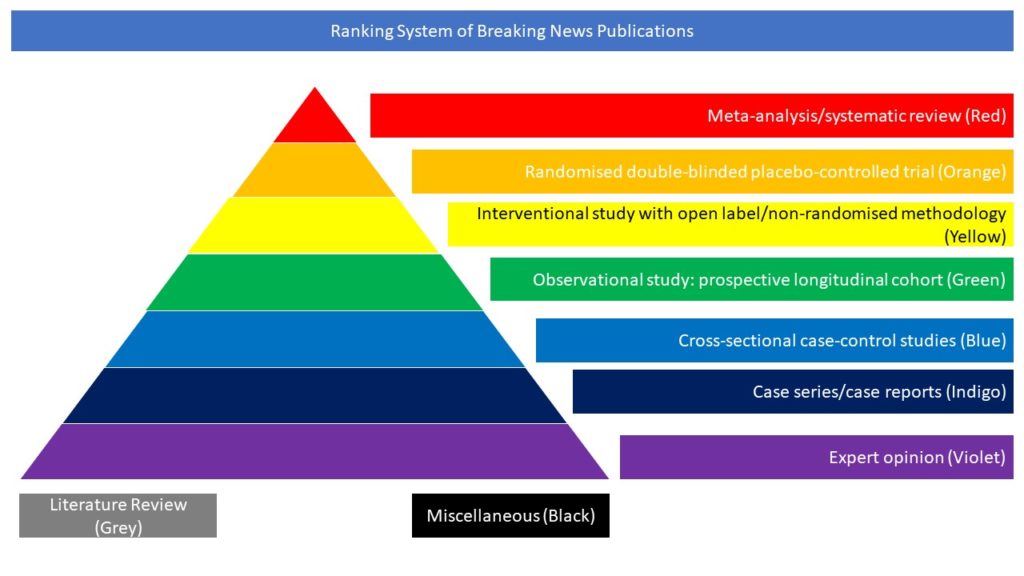
Interventional study with open label/non-randomised methodology (Yellow)
School-based COVID-19 contacts in England have been asked to self-isolate at home, missing key educational opportunities. In this study the authors trialled daily testing of contacts as an alternative to assess whether this resulted in similar control of transmission, while allowing more school attendance.
They performed an open-label, cluster-randomised, controlled trial in secondary schools and further education colleges in England. Schools were randomly assigned (1:1) to self-isolation of school-based COVID-19 contacts for 10 days (control) or to voluntary daily lateral flow device (LFD) testing for 7 days with LFD-negative contacts remaining at school (intervention). Randomisation was stratified according to school type and size, presence of a sixth form, presence of residential students, and proportion of students eligible for free school meals. Group assignment was not masked during procedures or analysis. Coprimary outcomes in all students and staff were COVID-19-related school absence and symptomatic PCR-confirmed COVID-19, adjusted for community case rates, to estimate within-school transmission (non-inferiority margin <50% relative increase). Analyses were done on an intention-to-treat basis using quasi-Poisson regression, also estimating complier average causal effects (CACE). Between March 18 and May 4, 2021, 204 schools were taken through the consent process, during which three decided not to participate further. 201 schools were randomly assigned (control group n=99, intervention group n=102) in the 10-week study (April 19–May 10, 2021), which continued until the pre-appointed stop date (June 27, 2021). 76 control group schools and 86 intervention group schools actively participated; additional national data allowed most non-participating schools to be included in analysis of coprimary outcomes. 2432 (42·4%) of 5763 intervention group contacts participated in daily contact testing. There were 657 symptomatic PCR-confirmed infections during 7 782 537 days-at-risk (59·1 per 100 000 per week) in the control group and 740 during 8 379 749 days-at-risk (61·8 per 100 000 per week) in the intervention group (intention-to-treat adjusted incidence rate ratio [aIRR] 0·96 [95% CI 0·75–1·22]; p=0·72; CACE aIRR 0·86 [0·55–1·34]). Among students and staff, there were 59 422 (1·62%) COVID-19-related absences during 3 659 017 person-school-days in the control group and 51 541 (1·34%) during 3 845 208 person-school-days in the intervention group (intention-to-treat aIRR 0·80 [95% CI 0·54–1·19]; p=0·27; CACE aIRR 0·61 [0·30–1·23]). The authors concluded that daily contact testing of school-based contacts was non-inferior to self-isolation for control of COVID-19 transmission, with similar rates of symptomatic infections among students and staff with both approaches. Infection rates in school-based contacts were low, with very few school contacts testing positive. Daily contact testing should be considered for implementation as a safe alternative to home isolation following school-based exposures.
Young BC, Eyre DW, Kendrick S, White C, Smith S, Beveridge G, Nonnenmacher T, Ichofu F, Hillier J, Oakley S, Diamond I, Rourke E, Dawe F, Day I, Davies L, Staite P, Lacey A, McCrae J, Jones F, Kelly J, Bankiewicz U, Tunkel S, Ovens R, Chapman D, Bhalla V, Marks P, Hicks N, Fowler T, Hopkins S, Yardley L, Peto TEA. Daily testing for contacts of individuals with SARS-CoV-2 infection and attendance and SARS-CoV-2 transmission in English secondary schools and colleges: an open-label, cluster-randomised trial. Lancet. 2021 Sep 14:S0140-6736(21)01908-5. doi: 10.1016/S0140-6736(21)01908-5.