by Elena R. Lebedeva
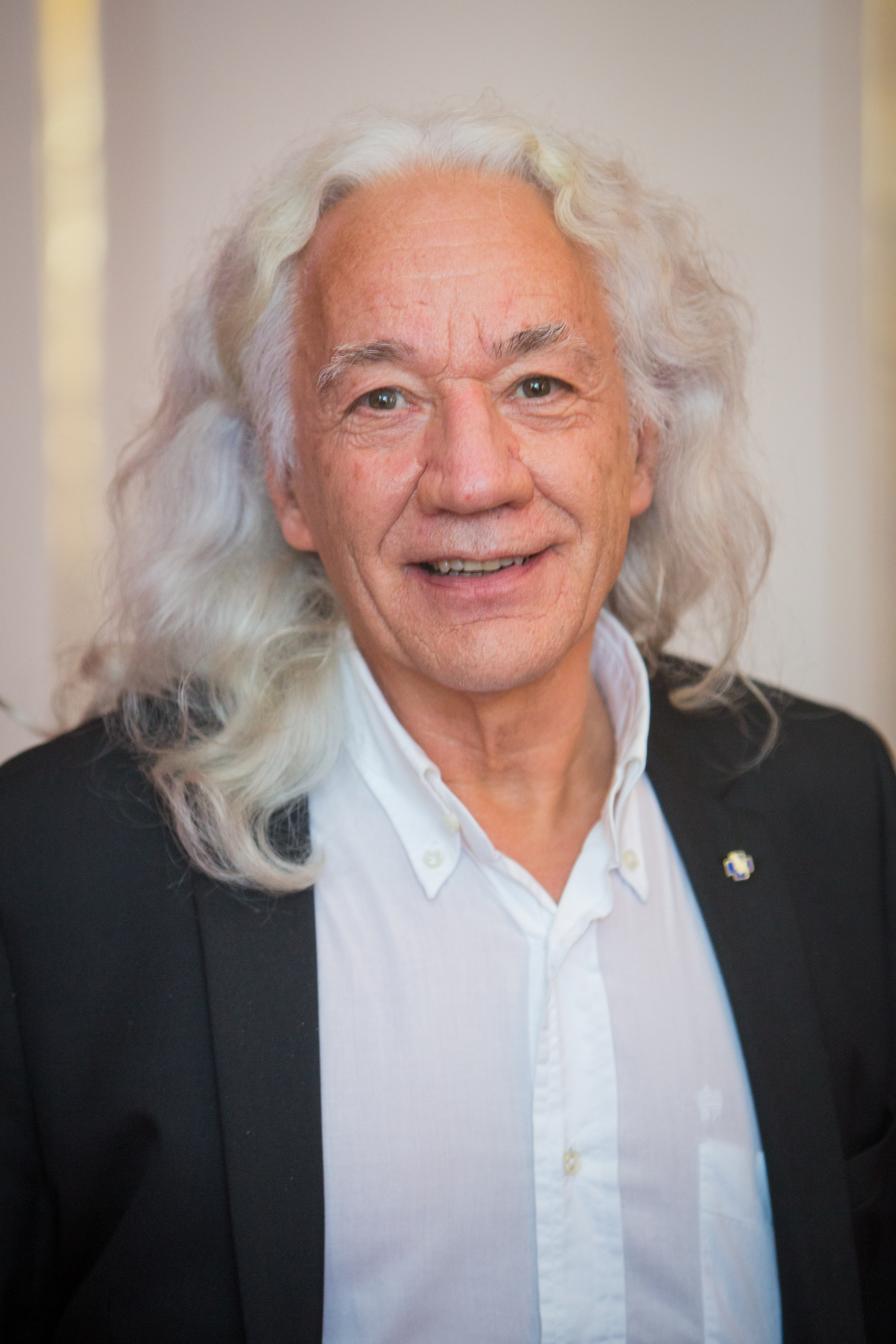
In March, Prof. David Dodick, Professor of Neurology, Director of the Headache and Concussion Programs at Mayo Clinic in Arizona, gave an excellent online presentation to the EAN Task Force on Gender and Diversity Issues in Neurology, detailing his successful strategies for large companies to reduce the burden of migraine among employees. Task Force member Prof. Elena Lebedeva, from the Ural State Medical University and International Headache Centre “Europe-Asia”, Yekaterinburg, Russia, followed up with an interview to get Dodick’s expert opinion on recent advances in headache treatment and management, including new possibilities for healthcare strategies to reduce the burden of migraine.
Elena Lebedeva: Prof. Dodick, you are one of the most recognised opinion leaders in the headache field. Which do you think are the most relevant advances in headache disorders?
David Dodick: Important question. Perhaps I will highlight what I think are five of the top recent advances.
First, the development of therapies that do not constrict blood vessels. Until recently, the belief that dilation of cerebral blood vessels was responsible for the headache pain of migraine drove the development of drugs for the acute treatment of migraine. This includes the triptans that were developed based on their ability to constrict extracranial and intracranial cerebral blood vessels. Over the past few years, two new classes of drugs have been approved that do not constrict blood vessels (gepants and ditans). Gepants target the calcitonin gene-related peptide (CGRP) receptor, and lasmiditan targets the serotonin (5HT)1F receptor, in contrast to triptans which target the 5HT1B and 5HT1D receptor. Unlike the 5HT1B receptor, the 5HT1F receptor is not located on blood vessels. This is an important advance for those with vascular disease or significant risk factors for vascular disease who cannot take triptans or ergots. It’s also important for those who do not respond to or tolerate triptans. Importantly, it also demonstrates how advances in our understanding of the mechanisms of disease can drive advances in treatment that are more disease-specific and mechanism-based. I should also point out that many of the new drugs and biologics that have been approved for migraine treatment may work outside the brain. The ability to terminate an individual attack as well as prevent their central generation with a drug that may work purely outside the brain, is a potentially very important advance and will no doubt teach us more about the biology of this disorder as well as inform future advances in treatment.
Second, almost every drug used for the acute treatment of migraine has the potential to produce maladaptive plasticity changes that can lead to medication overuse headache (MOH; aka rebound headache). However, gepants have been shown to be effective for both the acute and preventive treatment of migraine. If used daily or every other day, gepants actually reduce rather than increase the frequency of attacks. Preclinical animal models also support this clinical observation. CGRP appears from preclinical studies to be an important mediator of MOH, and this is reinforced from the observation that in clinical trials for the biologics (CGRP monoclonal antibodies) developed for migraine prevention, patients with chronic migraine even in the presence of medication overuse respond equally as well as those without medication overuse. Therefore, gepants may represent the first acute treatment for migraine that are not associated with MOH regardless of how often they’re used.
Third, the emergence of at least two neuropeptides that appear integral to the biology of a migraine attack is a major advance. One of these peptides – calcitonin gene-related peptide (CGRP) – and its receptor, are now the target of two drugs (gepants) and four biologics (monoclonal antibodies) that have been developed and approved for the preventive treatment of migraine (reduce the frequency of attacks) as well as for the treatment of an individual attack (acute treatment). There hasn’t been a single clinical trial testing these new therapies for the acute or preventive treatment of migraine that has failed to achieve the primary endpoint, and now, more than 1 million people across more than 45 countries have been treated with one or more of these new treatments. Pituitary adenylate-cyclase-activating polypeptide (PACAP) is the other promising peptide target for which a biologic is now in development.
Fourth, the identification of the hypothalamus as the likely site from which attacks are generated has already begun lines of investigation to dissect the cellular and molecular mechanisms by which attacks are generated. This includes investigations into the underlying mechanisms by which certain factors trigger migraine, including stress.
Fifth, the identification of the hypothalamus as being involved in the prodromal phase of the attack, has led to increasing focus on different phases of the attack, especially the prodromal phase, and to efforts to educate patients and clinicians to more carefully ask about and observe for symptoms of the prodromal phase (in much the same way we ask about an aura phase prior to epileptic seizures). Clinical trials evaluating therapies that are administered during the prodromal phase are underway. The early treatment of attacks before pain even begins could reduce the disability associated with attacks, the central sensitisation of pain pathways that occur as the attack progresses, and could reduce the risk of progression in some patients, though this will certainly require further studies. However, acute and preventive interventions that are deployed early in the attack and earlier before the disease becomes chronic, especially in those identified as being high risk for disease progression, is an important direction for the field.
EL: It is very important to destigmatise headache disorders among policymakers and the general public. Which strategies would you recommend?
DD: Migraine is the most common neurological disease in the world and accounts for more years lived with disability than any other disease that affects those under 50 years of age. The underlying biology and mechanisms of the disease are becoming elucidated, and this has led to tremendous advances in therapeutics which can reduce the burden of illness and change peoples’ lives. Now we need to educate the public, patients themselves, and policy makers on these facts. The strategies I would recommend are reflected in the initiatives I have helped lead over the past decade.
I have been involved in leading a major public awareness campaign in the United States, but with global reach. This is known as the “Move Against Migraine” campaign and is now in its 5th year. This has had a significant impact on the public’s understanding of migraine as a disabling neurological disease (with over 500,000 new visitors to its website each month over the past several years) and has been a tremendous source of support for patients. We hope this can serve as an inspiration and template for other headache advocacy organisations around the world.
ONE Neurology is another major public awareness campaign being led by the European Academy of Neurology and the European Federation of Neurological Associations. It is a collaboration of leading global advocacy organisations representing many neurological diseases. The ONE Neurology initiative aims to unite and strengthen neurologic-related groups to stimulate collaborative advocacy, action, and accountability for the prevention, treatment and management of neurological disorders worldwide. I am fortunate to be involved with this effort as well, representing the headache field, and this promises to destigmatise all neurological disorders including headache and migraine, and position them as a public health priority, especially since one in every three individuals is affected by a neurological disorder.
In a similar initiative that was global in scope and collaborative in nature, in 2017, as then President of the International Headache Society (IHS), we held the first IHS global patient advocacy summit (GPAS). This led to the formation of the International Headache Society’s Global Patient Advocacy Coalition (IHS-GPAC) – a global coalition of leading neurology, headache, and pain societies, patient advocacy organisations, and regulatory agencies. We have published the proceedings of two IHS-GPAS summits held in 2017 and 2019 known as the Vancouver Declaration. The Vancouver Declaration establishes advocacy goals and benchmarks and provides a blueprint for achieving advocacy goals in the field of headache. We have partnered with the World Federation of Neurology in dedicating (for the first time) World Brain Day 2019 to migraine and other headache disorders. We have also consulted with the World Health Organization and have since been working with global and regional employers to initiate migraine advocacy initiatives within the workplace. Since migraine impacts people during peak productive years while they are working and building careers, this seemed like a very good place to start. The goal of this programme is to educate employees with and without migraine, reduce the stigma associated with migraine in the workplace, empower patients to seek help, and improve the productivity of employees with migraine while reducing their burden of illness and improving their quality of life. IHS-GPAC has its sights set on several other advocacy initiatives that among others will prioritise students, teachers, and schools, as well as healthcare providers. For example, in August and September 2021, we have partnered with the African Academy of Neurology and the World Federation of Neurology to provide headache education to healthcare providers in Africa in an effort to raise the level of care for people in Africa impacted by headache disorders.
Advocacy for research to continue to drive advances in knowledge and treatment is another very important advocacy domain. As chair of the American Brain Foundation, we have also highlighted headache disorders as one of many neurological disorders that needs further research. To this end, we have established and endowed a headache research fund that will soon begin to fund the best research in the field.
What these efforts highlight is that there are numerous advocacy domains that require attention but that with a tenacious commitment to the cause and a true collaboration that is multi-stakeholder and involves patients, patient organisations, clinician and scientist leaders, professional societies, NGOs, and regulators, we can and we will destigmatise headache disorders and all neurological disorders, ensure access to care and essential medicines, and ultimately prevent disease, reduce the burden of illness, and improve an affected person’s quality of life.
EL: You have developed specific and successful strategies to help employers to reduce the burden of migraine between employees. Can you tell us something more about that?
DD: Yes, first in a study supported by the International Headache Society and the World Health Organization Western Pacific Region Office, we assessed the prevalence, characteristics, and disability of headache disorders at a Japanese information technology company. What we found was that 17% had migraine and the disease burden among these employees was associated with substantial losses in productivity and employer cost. These results supported the development and implementation of workplace programmes and in collaboration with the Japanese Headache Society and Japanese Patient Advocacy Coalition, IHS-GPAC successfully implemented an employee programme to reduce stigma associated with migraine in the workplace, improve migraine management in the workplace, and reduce the burden and costs associated with lost workplace productivity. We have now used this as a model and template to extend this employee migraine programme to other global, national and regional employers throughout the world. Since the prevalence of migraine is highest between the ages 18-55, we felt that we could make a significant impact on stigma and the care of people with migraine by focusing on the workplace. We have been overwhelmed at the receptiveness and positive response from employers – large and small – in wanting to improve the health-related quality of life of their employees.
EL: Sex differences are very important in the headache field. Do you think they are adequately addressed or there are still some gaps?
DD: There are definitely still some gaps that need to be closed. In fact, part of the stigma surrounding migraine and other headache disorders rests on the fact that they predominantly affect women. Of the more than 39 million Americans for example with migraine, more than 73% are women. The exciting fact is that we are now uncovering some of the fundamental biological mechanisms that account for why headache disorders are so much more common in women. We need to double down on our educational efforts to explain the sexually dimorphic nature of migraine and other pain syndromes, eliminate this stigma, and help both the public and clinicians understand how the differences in biology will actually be utilised to drive advances in treatment.
Migraine is one reason why some women are not gainfully employed. While significantly more women have entered the workplace, currently, the labour force participation rate of prime working-age women—those between the ages of 25 and 54— is at 74%, compared with over 93% for prime working-age men. Employees with chronic migraine reported being more worried about long-term financial security and covering living expenses and that their career advancement had been strained as a result of migraine. Due to the lack of understanding of what migraine is and how disabling it can be, women with migraine also face serious discrimination in the workplace and may be labelled as being less dependable because of what is perceived to be “just a headache”. This stigma can result in significant stress and guilt and lead to a worsening of their underlying condition. The IHS-GPAC employee programme should reduce the stigma around migraine directed toward women and lead to the necessary accommodations to empower women in the workplace to take control of this illness and seek the help they need so that their quality of work-life and productivity are maximised.
Ultimately, I see public and workplace advocacy focused on migraine – the most common neurological disorder affecting women in the world – as a public health priority for women both inside and outside schools and the workplace, and a strategy to ensure that women can pursue and achieve their educational and career aspirations without restraint, stigma, or discrimination.