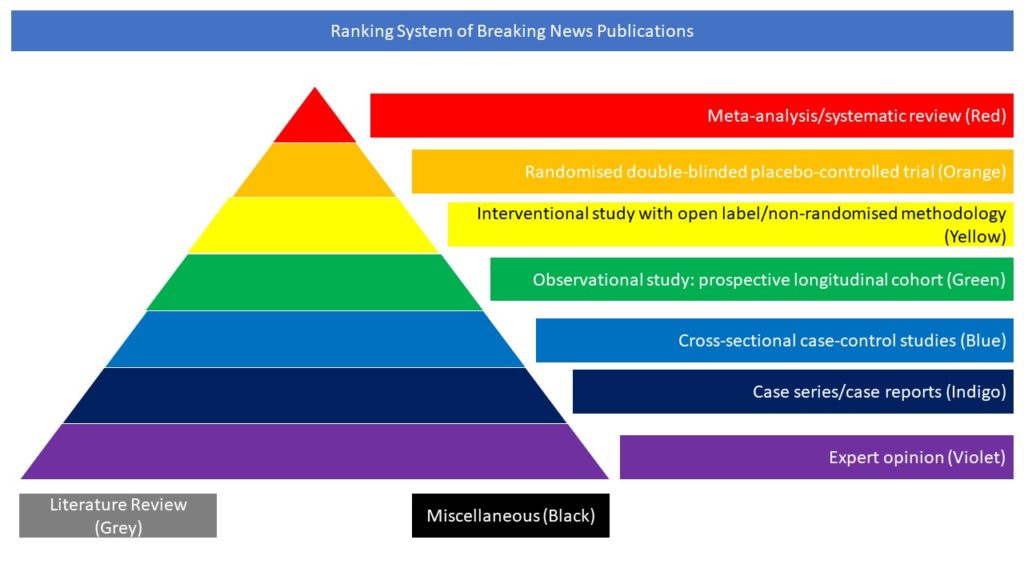
Interventional study with open label/non-randomised methodology (Yellow)
SARS-CoV-2 entry in human cells depends on angiotensin-converting enzyme 2, which can be upregulated by inhibitors of the renin–angiotensin system (RAS). In this article the authors aimed to test the hypothesis that discontinuation of chronic treatment with ACE-inhibitors (ACEIs) or angiotensin II receptor blockers (ARBs) mitigates the course of recent-onset COVID-19.
ACEI-COVID was a parallel group, randomised, controlled, open-label trial done at 35 centres in Austria and Germany. Patients aged 18 years and older were enrolled if they presented with recent symptomatic SARS-CoV-2 infection and were chronically treated with ACEIs or ARBs. Patients were randomly assigned 1:1 to discontinuation or continuation of RAS inhibition for 30 days. Primary outcome was the maximum sequential organ failure assessment (SOFA) score within 30 days, where death was scored with the maximum achievable SOFA score. Secondary endpoints were area under the death-adjusted SOFA score (AUCSOFA), mean SOFA score, admission to the intensive care unit, mechanical ventilation, and death. Analyses were done on a modified intention-to-treat basis.
Between April 20, 2020, and Jan 20, 2021, 204 patients (median age 75 years [IQR 66–80], 37% females) were randomly assigned to discontinue (n=104) or continue (n=100) RAS inhibition. Within 30 days, eight (8%) of 104 died in the discontinuation group and 12 (12%) of 100 patients died in the continuation group (p=0·42). There was no significant difference in the primary endpoint between the discontinuation and continuation group (median [IQR] maximum SOFA score 0·00 (0·00–2·00) vs 1·00 (0·00–3·00); p=0·12). Discontinuation was associated with a significantly lower AUCSOFA (0·00 [0·00–9·25] vs 3·50 [0·00–23·50]; p=0·040), mean SOFA score (0·00 [0·00–0·31] vs 0·12 [0·00–0·78]; p=0·040), and 30-day SOFA score (0·00 [10–90th percentile, 0·00–1·20] vs 0·00 [0·00–24·00]; p=0·023). At 30 days, 11 (11%) in the discontinuation group and 23 (23%) in the continuation group had signs of organ dysfunction (SOFA score ≥1) or were dead (p=0·017). There were no significant differences for mechanical ventilation (10 (10%) vs 8 (8%), p=0·87) and admission to intensive care unit (20 [19%] vs 18 [18%], p=0·96) between the discontinuation and continuation group. The authors concluded that discontinuation of RAS-inhibition in COVID-19 had no significant effect on the maximum severity of COVID-19 but may lead to a faster and better recovery. The decision to continue or discontinue should be made on an individual basis, considering the risk profile, the indication for RAS inhibition, and the availability of alternative therapies and outpatient monitoring options.
Bauer A, Schreinlechner M, Sappler N, Dolejsi T, Tilg H, Aulinger BA, Weiss G, Bellmann-Weiler R, Adolf C, Wolf D, Pirklbauer M, Graziadei I, Gänzer H, von Bary C, May AE, Wöll E, von Scheidt W, Rassaf T, Duerschmied D, Brenner C, Kääb S, Metzler B, Joannidis M, Kain HU, Kaiser N, Schwinger R, Witzenbichler B, Alber H, Straube F, Hartmann N, Achenbach S, von Bergwelt-Baildon M, von Stülpnagel L, Schoenherr S, Forer L, Embacher-Aichhorn S, Mansmann U, Rizas KD, Massberg S; ACEI-COVID investigators. Discontinuation versus continuation of renin-angiotensin-system inhibitors in COVID-19 (ACEI-COVID): a prospective, parallel group, randomised, controlled, open-label trial. Lancet Respir Med. 2021 Jun 11:S2213-2600(21)00214-9. doi: 10.1016/S2213-2600(21)00214-9