By Ulf Kallweit
“Sleep is by the brain (…) and for the brain” (Hobson, 2005).
Narcolepsy is a rare brain disorder and is also a model disease for the understanding of sleep and wake regulation mechanisms and of their pathology.
Excessive daytime sleepiness, cataplexy and REM-associated phenomena are primary symptoms of narcolepsy. They result in a limitation of performance, ability to work, and quality of life of affected patients.
An updated guideline is needed since knowledge on the etiopathology and on the clinical characteristics has significantly increased in recent years, along with the availability of several new drugs. These advancements allow, for the first time, individualised management of patients.
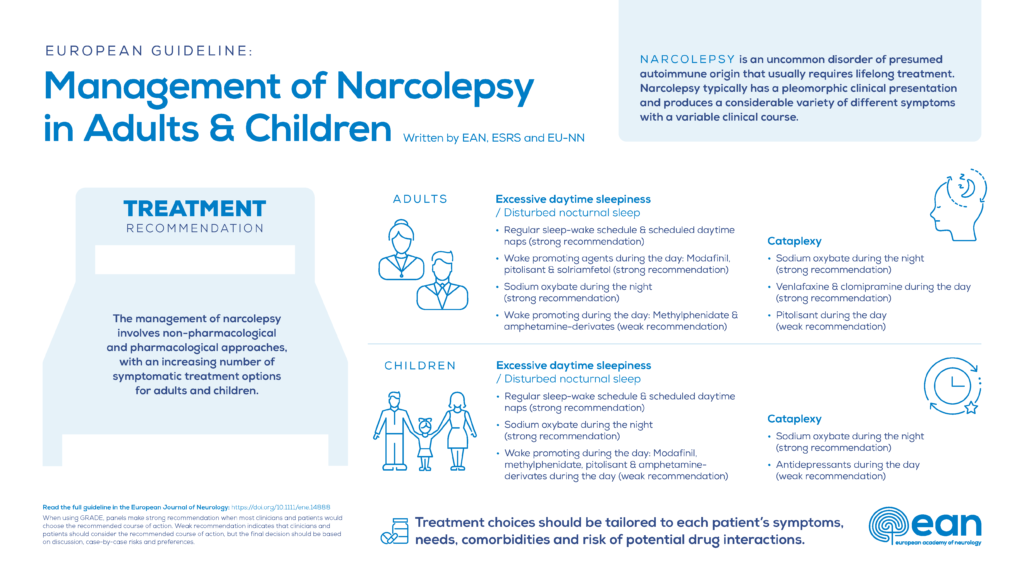
We, European narcolepsy experts nominated by the European Academy of Neurology (EAN), European Sleep Research Society (ESRS) and European Narcolepsy Network (EU-NN), joined forces, together with patient representatives, in order to provide an up-to-date, evidence-based guideline for the treatment of narcolepsy.
When evidence for recommendations was limited, we provided statements in order to give a complete guideline, covering all aspects necessary for clinical management.
In our guideline we applied the PICO (Patients–Intervention–Comparator–Outcome) framework and formulated key questions relevant for the clinical management of patients. For example, one questions was:
“What is the clinical evidence for efficacy of pharmacological treatment of moderate to severe cataplexy in adults?” We answered this question by giving an overview of recommendations (in this case: strong recommendations for sodium oxybate, venlafaxine, clomipramine, and a weak recommendation for pitolisant). We also provide the corresponding level of evidence and references.
We believe this guideline will be useful for neurologists and sleep specialists in their daily clinical care of narcolepsy patients and will help to improve patients’ lives.
***
Abstract
Background and aim
Narcolepsy is an uncommon hypothalamic disorder of presumed autoimmune origin that usually requires lifelong treatment. This paper aims to provide evidence-based guidelines for the management of narcolepsy in both adults and children.
Methods
The European Academy of Neurology (EAN), European Sleep Research Society (ESRS) and European Narcolepsy Network (EU-NN) nominated a task force of 18 narcolepsy specialists. According to the EAN recommendations, 10 relevant clinical questions were formulated in PICO format. Following a systematic review of the literature (performed in Autumn 2018 and updated in July 2020) recommendations were developed according to the GRADE approach.
Results
A total of 10,247 references were evaluated, 308 studies were assessed and 155 finally included. The main recommendations can be summarised as follows: (i) excessive daytime sleepiness in adults—scheduled naps, modafinil, pitolisant, sodium oxybate (SXB), solriamfetol (all strong), methylphenidate, amphetamine derivates (both weak); (ii) cataplexy in adults—SXB, venlafaxine, clomipramine (all strong) and pitolisant (weak); (iii) excessive daytime sleepiness in children—scheduled naps, SXB (both strong), modafinil, methylphenidate, pitolisant, amphetamine derivates (all weak); (iv) cataplexy in children—SXB (strong), antidepressants (weak). Treatment choices should be tailored to each patient’s symptoms, comorbidities, tolerance and risk of potential drug interactions.
Conclusion
The management of narcolepsy involves non-pharmacological and pharmacological approaches with an increasing number of symptomatic treatment options for adults and children that have been studied in some detail.
First published: 25 June 2021 https://doi.org/10.1111/ene.14888












