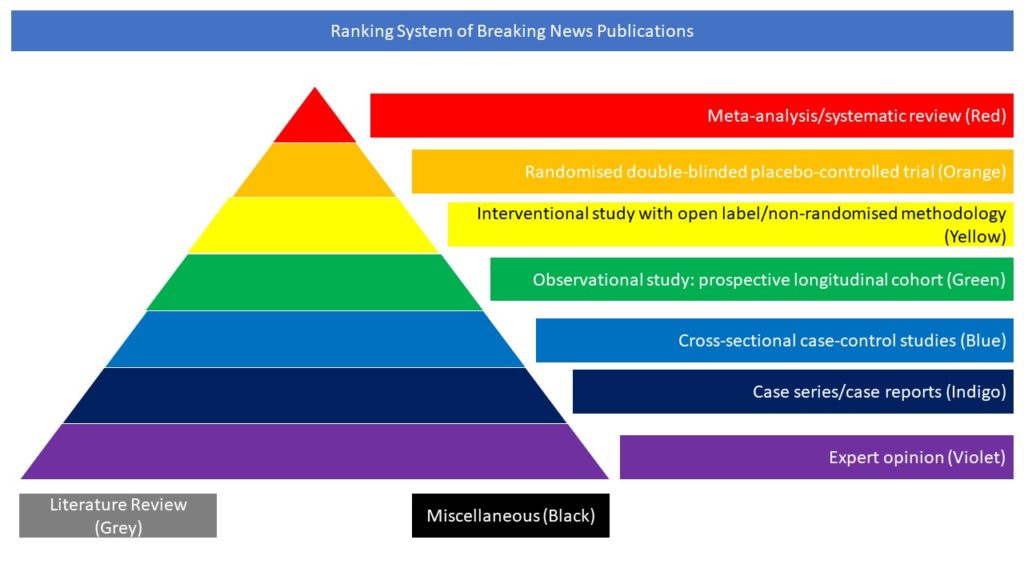
Cross-sectional case-control studies (Blue)
COVID‐19 affects the brain in various ways, among which delirium is worrying. In this article, the authors assessed whether a specific, long‐lasting, COVID‐19‐related brain injury develops in acute respiratory distress syndrome patients after life‐saving re‐oxygenation. Ten COVID+ patients (COVID+) with unusual delirium associated with neuroimaging suggestive of diffuse brain injury, and seven controls with non‐COVID encephalopathy were studied. The assessment took place when the intractable delirium started at weaning off ventilation support. Brain magnetic resonance imaging (MRI), followed by standard cerebrospinal fluid (CSF)‐analyses and assessment of CSF‐erythropoietin (EPO) concentrations (as a marker for the assessment of tissue repair), and of non‐targeted CSF‐metabolomics using LC‐HR‐mass spectrometry were performed. Patients were similar as regards severity scores, but COVID+ patients were hospitalised for longer (25 [11.75; 25] versus 9 [4.5; 12.5] days, p=0.03). On admission, but not at MRI and lumbar puncture performance, COVID+ were more hypoxic (p=0.002). On MRI, leptomeningeal enhancement and diffuse white matter haemorrhages were seen only in COVID+ patients. In the latter, CSF‐EPO concentration was lower (1.73 [1.6; 2.06] versus 3.04 [2.9; 3.91] mUI/ml, p= 0.01), and CSF‐metabolomics indicated: a) increased compounds such as foodborne molecules (sequiterpenes), molecules from industrialised beverages, and micro‐pollutants (di‐ethanolamine); b) decreased molecules as incomplete breakdown‐products of protein catabolism, and foodborne molecules (glabridin). At 3‐month discharge, fatigue, anxiety and depression as well as MRI lesions persisted in COVID+ patients. The authors concluded that some COVID+ patients are at risk of a specific delirium syndrome. Imperfect brain repair after re‐oxygenation and lifestyle factors might influence long‐lasting brain injuries in a context of foodborne micro‐pollutants.