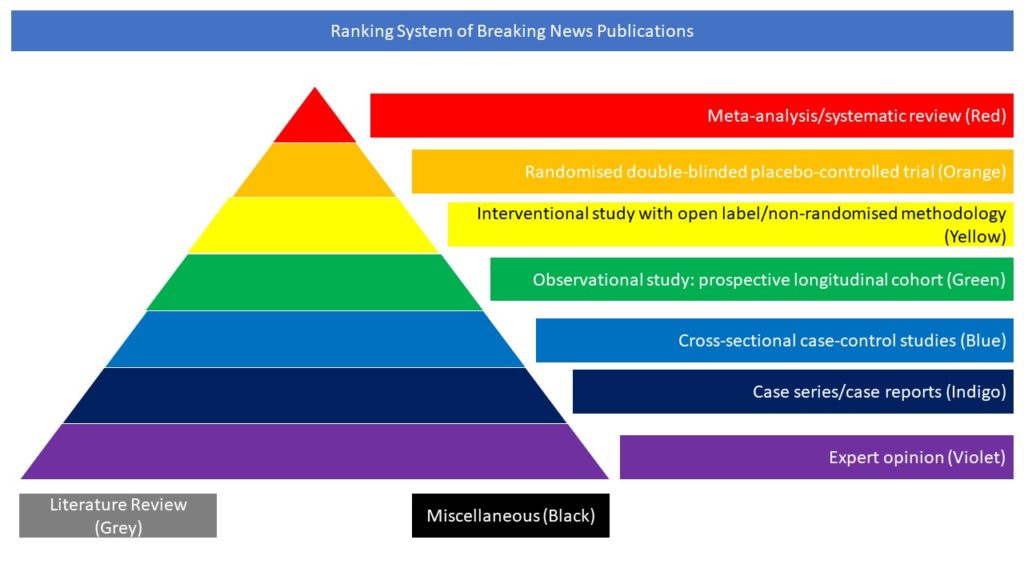
Interventional study with open label/non-randomised methodology (Yellow)
The objective of this randomised, open label trial was to determine whether tocilizumab improves clinical outcomes for patients with severe or critical COVID-19. Adults with confirmed COVID-19 who were receiving supplemental oxygen or mechanical ventilation and had abnormal levels of at least two serum biomarkers (C reactive protein, D dimer, lactate dehydrogenase, or ferritin) were recruited from nine hospitals in Brazil, 8 May to 17 July 2020. The data monitoring committee recommended stopping the trial early, after 129 patients had been enrolled, because of an increased number of deaths at 15 days in the tocilizumab group. Tocilizumab (single intravenous infusion of 8 mg/kg) plus standard care (n=65) was compared to standard care alone (n=64). The primary outcome, clinical status measured at 15 days using a seven level ordinal scale, was analysed as a composite of death or mechanical ventilation because the assumption of odds proportionality was not met. A total of 129 patients were enrolled (mean age 57 (SD 14) years; 68% men) and all completed follow-up. All patients in the tocilizumab group and two in the standard care group received tocilizumab. 18 of 65 (28%) patients in the tocilizumab group and 13 of 64 (20%) in the standard care group were receiving mechanical ventilation or died at day 15 (odds ratio 1.54, 95% confidence interval 0.66 to 3.66; P=0.32). Death at 15 days occurred in 11 (17%) patients in the tocilizumab group compared with 2 (3%) in the standard care group (odds ratio 6.42, 95% confidence interval 1.59 to 43.2). Adverse events were reported in 29 of 67 (43%) patients who received tocilizumab and 21 of 62 (34%) who did not receive tocilizumab. The authors concluded that in patients with severe or critical COVID-19, tocilizumab plus standard care was not superior to standard care alone in improving clinical outcomes at 15 days, and it might increase mortality.