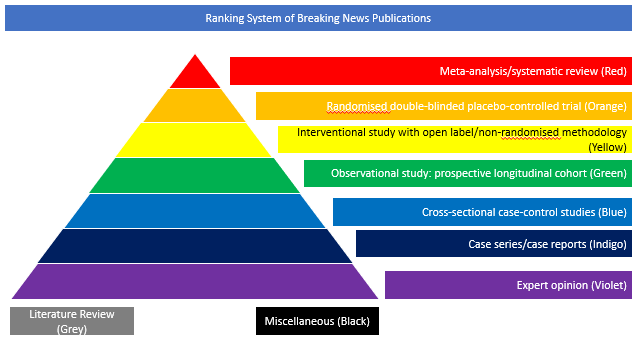
Cross-sectional case-control studies (Blue)
Biological data are lacking with respect to risk of vertical transmission and mechanisms of fetoplacental protection in maternal SARS-CoV-2 infection. The objective of this cohort study was
to quantify SARS-CoV-2 viral load in maternal and neonatal biofluids, transplacental passage of anti–SARS-CoV-2 antibody, and incidence of fetoplacental infection. The study was conducted among pregnant women presenting to 3 tertiary care centres in Boston, Massachusetts. Women with RT-PCR results positive for SARS-CoV-2 were recruited from April 2 to June 13, 2020, and follow-up occurred through July 10, 2020. Contemporaneous participants without SARS-CoV-2 infection were enrolled as a convenience sample from pregnant women with RT-PCR results negative for SARS-CoV-2. The main outcomes were SARS-CoV-2 viral load in maternal plasma or respiratory fluids and umbilical cord plasma, quantification of anti–SARS-CoV-2 antibodies in maternal and cord plasma, and presence of SARS-CoV-2 RNA in the placenta. Among 127 pregnant women enrolled, 64 with RT-PCR results positive for SARS-CoV-2 (mean [SD] age, 31.6 [5.6] years) and 63 with RT-PCR results negative for SARS-CoV-2 (mean [SD] age, 33.9 [5.4] years) provided samples for analysis. Of women with SARS-CoV-2 infection, 23 (36%) were asymptomatic, 22 (34%) had mild disease, 7 (11%) had moderate disease, 10 (16%) had severe disease, and 2 (3%) had critical disease. In viral load analyses among 107 women, there was no detectable viraemia in maternal or cord blood and no evidence of vertical transmission. Among 77 neonates tested in whom SARS-CoV-2 antibodies were quantified in cord blood, 1 had detectable immunoglobulin M to nucleocapsid. Among 88 placentas tested, SARS-CoV-2 RNA was not detected in any. In antibody analyses among 37 women with SARS-CoV-2 infection, anti–receptor binding domain immunoglobin G was detected in 24 women (65%) and anti-nucleocapsid was detected in 26 women (70%). Mother-to-neonate transfer of anti–SARS-CoV-2 antibodies was significantly lower than transfer of anti-influenza hemagglutinin A antibodies (mean [SD] cord-to-maternal ratio: anti–receptor binding domain immunoglobin G, 0.72 [0.57]; anti-nucleocapsid, 0.74 [0.44]; anti-influenza, 1.44 [0.80]; P < .001). Non-overlapping placental expression of SARS-CoV-2 receptors angiotensin-converting enzyme 2 and transmembrane serine protease 2 was noted. In this cohort study, there was no evidence of placental infection or definitive vertical transmission of SARS-CoV-2. Transplacental transfer of anti-SARS-CoV-2 antibodies was inefficient. Lack of viraemia and reduced coexpression and colocalisation of placental angiotensin-converting enzyme 2 and transmembrane serine protease 2 may serve as protective mechanisms against vertical transmission.
doi: 10.1001/jamanetworkopen.2020.30455