By Karin Klijn
By Karin Klijn
Over the past three decades the diagnosis and treatment of stroke has seen tremendous changes, which have led to a complete change of clinical practice, probably best illustrated by the adagio “time is brain”.
Dutch researchers have been deeply involved in the progress that has been achieved in this era of evidence-based medicine. From the early days on they have been either leading in national and international randomized clinical trials on stroke treatment and secondary prevention or participating in landmark international trials led by their international collaborators. Their interest has spanned the full range of neurovascular disorders, including ischemic stroke, intracerebral and subarachnoid hemorrhage, and cerebral venous sinus thrombosis. In addition, Dutch researchers have been at the forefront of the development of evidence-based rehabilitation strategies after stroke.

 As early as 1984, Rien Vermeulen and Jan van Gijn, together with colleagues from UK and Sweden, reported that in patients with aneurysmal subarachnoid hemorrhage antifibrinolytic treatment with tranexamic acid reduced the number of patients with re-bleeding, although with the cost of inducing delayed cerebral ischemia (Vermeulen et al. N Eng J Med 1984). In the ‘90s, three large secondary prevention trials after TIA or minor ischemic stroke were completed: the Dutch TIA trial, led by Ale Algra and Jan van Gijn (Dutch TIA Trial Study Group. N Eng J Med 1991), the European Atrial Fibrillation Trial, led by Peter Koudstaal (EAFT study group. Lancet 1993), and the SPIRIT trial, led by Ale Algra (SPIRIT Study Group. Ann Neurol 1997). Results of these trials are still visible in the current secondary preventive treatment of patients with TIA and ischemic stroke around the world. In addition, the cerebral venous sinus thrombosis trial led by Jan Stam showed that in patients with cerebral venous sinus thrombosis, treatment with low-molecular-weight heparin followed by oral anticoagulation was safe, even in patients with cerebral hemorrhage (de Bruijn et al. Stroke 1999).
As early as 1984, Rien Vermeulen and Jan van Gijn, together with colleagues from UK and Sweden, reported that in patients with aneurysmal subarachnoid hemorrhage antifibrinolytic treatment with tranexamic acid reduced the number of patients with re-bleeding, although with the cost of inducing delayed cerebral ischemia (Vermeulen et al. N Eng J Med 1984). In the ‘90s, three large secondary prevention trials after TIA or minor ischemic stroke were completed: the Dutch TIA trial, led by Ale Algra and Jan van Gijn (Dutch TIA Trial Study Group. N Eng J Med 1991), the European Atrial Fibrillation Trial, led by Peter Koudstaal (EAFT study group. Lancet 1993), and the SPIRIT trial, led by Ale Algra (SPIRIT Study Group. Ann Neurol 1997). Results of these trials are still visible in the current secondary preventive treatment of patients with TIA and ischemic stroke around the world. In addition, the cerebral venous sinus thrombosis trial led by Jan Stam showed that in patients with cerebral venous sinus thrombosis, treatment with low-molecular-weight heparin followed by oral anticoagulation was safe, even in patients with cerebral hemorrhage (de Bruijn et al. Stroke 1999).
Many of us, as Dutch stroke researchers of the current century, have benefited from the mentorship and leading example of the stroke-researchers of the first hours. As a result, many more randomized clinical trials (eg. ESPRIT, SICHPA, HAMLET, MASH, ARTIS, PAIS, PASS, PATCH) as well as valuable etiological, diagnostic and prognostic studies have been completed since.
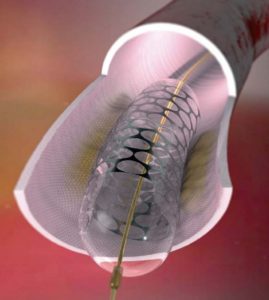
 In 2014, stroke research in The Netherlands resulted in the completion of the MrClean trial. The MrClean trial was the first trial demonstrating that in patients with acute ischemic stroke caused by a proximal intracranial arterial occlusion of the anterior circulation, intra-arterial treatment administered within 6 hours leads to better functional recovery after three months without increasing case-fatality (Berkhemer et al. N Eng J Med 2015).
In 2014, stroke research in The Netherlands resulted in the completion of the MrClean trial. The MrClean trial was the first trial demonstrating that in patients with acute ischemic stroke caused by a proximal intracranial arterial occlusion of the anterior circulation, intra-arterial treatment administered within 6 hours leads to better functional recovery after three months without increasing case-fatality (Berkhemer et al. N Eng J Med 2015).
 Presentation of the results of the MrClean trial received an overwhelming standing ovation of the audience at the World Stroke Conference in Istanbul. The MrClean trial exemplifies how close and multidisciplinary collaboration between specialists in both university and non-university hospitals in The Netherlands can lead to major improvement in stroke treatment. The Dutch stroke research community has united in the CONTRAST consortium (consortium for new treatments of acute stroke) with the aim to continue to improve outcome after acute stroke. Over the next five years, the CONTRAST consortium will perform five new large acute stroke trials testing novel treatment strategies in ischemic stroke and intracerebral hemorrhage, it will identify patients who will benefit most from these interventions through advanced imaging, and it will elucidate mechanisms of incomplete microvascular reperfusion with a view to developing new treatments.
Presentation of the results of the MrClean trial received an overwhelming standing ovation of the audience at the World Stroke Conference in Istanbul. The MrClean trial exemplifies how close and multidisciplinary collaboration between specialists in both university and non-university hospitals in The Netherlands can lead to major improvement in stroke treatment. The Dutch stroke research community has united in the CONTRAST consortium (consortium for new treatments of acute stroke) with the aim to continue to improve outcome after acute stroke. Over the next five years, the CONTRAST consortium will perform five new large acute stroke trials testing novel treatment strategies in ischemic stroke and intracerebral hemorrhage, it will identify patients who will benefit most from these interventions through advanced imaging, and it will elucidate mechanisms of incomplete microvascular reperfusion with a view to developing new treatments.
We look forward to seeing you at the EAN in Amsterdam.
References:
- Antifibrinolytic treatment in subarachnoid hemorrhage; Vermeulen M, Lindsay KW, Murray GD, Cheah F, Hijdra A, Muizelaar JP, Schannong M, Teasdale GM, van Crevel H, van Gijn J..N Engl J Med. 1984;311:432-7.
- The Dutch TIA Trial Study Group. A comparison of two doses of aspirin (30 mg vs. 283 mg a day) in patients after a transient ischemic attack or minor ischemic stroke. N Engl J Med. 1991;32:1261-6.
- European Atrial fibrillation Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. Lancet 1993;342:1255-62.
- The Stroke Prevention in Reversible Ischemia Trial (SPIRIT) Study Group. A randomized trial of anticoagulants versus aspirin after cerebral ischemia of presumed arterial origin. Ann Neurol. 1997;42:857-65.
- Randomized, placebo-controlled trial of anticoagulant treatment with low-molecular-weight heparin for cerebral sinus thrombosis; de Bruijn SFTM, Stam J, for the Cerebral Venous Sinus Thrombosis Study Group.. Stroke. 1999;30:484-8.
- A randomized trial of intraarterial treatment for acute ischemic stroke; Berkhemer et al.. N Eng J Med. 2015;372:11-20.
Dr. Karin Klijn works at the Radboud University Medical Center – Department of Neurology, Nijmegen