Ahmed Abbas, London, UK
Term of Fellowship: August – November 2023
Hosting department: Brain Center UMC Utrecht, Department of Neurology and Neurosurgery, University Medical Centre Utrecht, The Netherlands
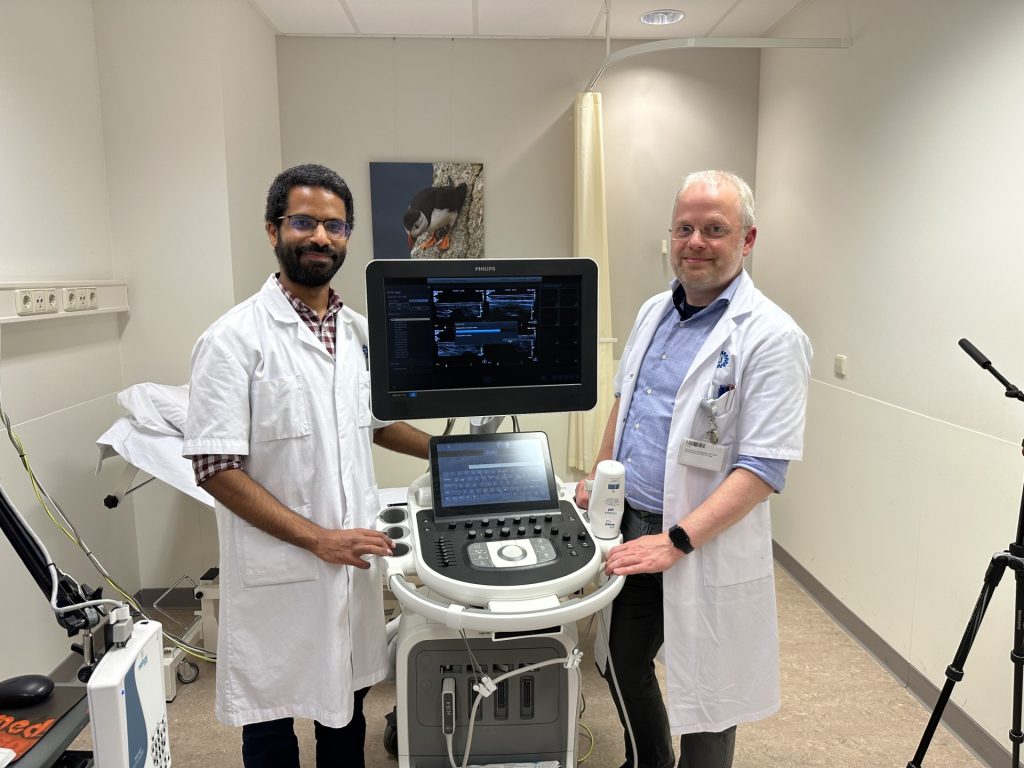
Supervisor: Dr Stephan Goedee
…
I am very grateful to the European Academy of Neurology for making possible a wonderful 12-week Clinical Fellowship at the University Medical Centre Utrecht with Dr Stephan Goedee and his colleagues.
I was attracted to Utrecht by the wealth of neuromuscular ultrasound experience, especially as applied to inflammatory neuropathies, where it has really been pioneered by Dr Goedee. When I first arrived, I had barely ever held an ultrasound probe in my hand, however by the final week I was effectively flying solo, except for the occasional supervisory glances over my shoulder.
Dr Goedee arranged a graduated and structured programme in which I could learn this imaging technique. In the early days, it was useful to largely observe ultrasound studies being performed. Many staff members then walked in on me undertaking ultrasound on my own leg/arm/neck nerves (may I take this opportunity to apologise to any who may have developed PTSD!), and several technicians in the department also kindly offered up their own limbs for practice. I quickly progressed to scanning actual patients, initially focusing on relatively straightforward protocols (e.g. carpal tunnel screening) and steadily progressing to more complex structures such as the nerve roots and brachial plexus in inflammatory neuropathies.
A particularly valuable learning opportunity took place in the Inflammatory Neuropathy clinic on Tuesdays. Many follow-up patients with known CIDP or MMN would very kindly stay behind after their neurology clinic appointment, so that I could perform ultrasound on them for my own learning. This allowed me to acquire a substantial amount of inflammatory neuropathy imaging experience in a relatively condensed period.
Neuromuscular ultrasound has increasingly emerged as a useful tool complementing nerve conduction studies, not only in the setting of inflammatory neuropathies, but also in other areas such as peripheral nerve entrapments, trauma or tumours. I was exposed to all of these different pathologies, and I am planning on incorporating the imaging skills acquired in this fellowship into my own clinical practice in the UK.
Although not the primary aim of my fellowship, it was also a fantastic opportunity to engage in further learning in the field of nerve conduction studies and electromyography. For example, the local protocols in Utrecht for assessment of suspected MMN are very extensive, and certainly more than I would have otherwise routinely undertaken. Similarly, I enjoyed sitting in several inflammatory neuropathy, myopathy and motor neuron clinics. The department also has a very strong basic and clinical research track record and a vibrant Friday academic programme.
Outside of work it was so wonderful exploring Utrecht and several other cities in the beautiful country that is the Netherlands. On one occasion, Dr Goedee and I suddenly found ourselves discussing nerve-related matters during a short break in an orchestral performance, so we very wisely decided to steer the conversation in a different direction, at least for that evening!
Finally, I want to extend my sincere thanks in particular to Dr Goedee, and more widely also to his colleagues, for everything I have learned. It was a real pleasure spending time in their warm and welcoming department. I will treasure my EAN Clinical Fellowship experience.
Matthias De Wachter, Antwerp, Belgium
Term of Fellowship: October – December 2023
Hosting department: Filadelfia Epilepsy Hospital, Dianalund, Denmark
Supervisor: Prof. Rikke Steensbjerre Møller
…
Before my departure to Filadelfia Epilepsy Center, my goals were to augment my knowledge of genetic epilepsies: starting from interpreting genetic results, over phenotyping and links with EEG to treatment implications. With this EAN Clinical Fellowship I mainly had the goal to learn skills that could be used in clinical practice later.
During my stay, I have been able to come in contact with all these different aspects.
The first interesting thing I encountered was the unique setting of Filadelfia Epilepsy Center.
As a national reference centre of epilepsy in Denmark, it is the only centre in Denmark that offers high-specialised care for patients with epilepsy. Because of its unique position, it has patients from all over the country, and with different rare genetic epilepsies. I was part of a highly experienced team, both in clinical practice as well as in research. The unique aspects of having different specialities in one department, even in one hallway, made it particularly interesting. Specialised nurses, a pharmacist, a genetic technician, geneticists and (child) neurologists are working closely together.
To learn more about genetic epilepsies, I was asked to focus on a few genes, to get to know them as well as possible. I focused on the clinical aspects of KCNQ2/3 (gain of function) and KCNA2 gain of function. I looked into the phenotype, but more importantly into the treatment responses to targeted treatments. To achieve this, I had several encounters with parents of patients and clinicians involved in the clinical care of these patients. I can truly say that this was a great experience. Not only did I learn a lot of these genes and their functions, but I learned a lot from the clinical aspects, which I can take back to my own clinical practice in Belgium.
I also had the chance to see patients in a residential setting, as they were admitted for diagnostic or therapeutic work-up. It reminded me about a rotation I did during my residencies in the rehabilitation centre of Pulderbos. Observing children in an out-of-hospital environment, where they can play and interact with other children, is of additional value for a young clinician like me. It gives you the opportunity to observe their general functioning, and it reminded me how important it is for us, as clinicians, to look beyond seizures.
Apart from these clinical and scientific experiences, I was also able to extent my knowledge in other ways. We visited the genetic lab with the whole team, taking us back to the basics of genetic testing and we had a teaching session on the interpretation of genetic variants. We visited Stockholm for a special teaching course on genetic epilepsies for clinicians, which included practical workshops on how to go from the genetic report to treatment. And I attended, thanks to the support of the department, meetings in Oslo, Copenhagen and Rome, all clinical-oriented conferences, allowing me to present our work. I must say that I have extended my network a lot, which allows me to improve my clinical practice at home.
Apart from my professional experience, I had a wonderful time just being in Denmark. My family joined me on this adventure, and our daughter enjoyed the ‘Northern’ experience a lot. I have made new friends from all over the world, and I already look forward to meeting them at international events and conferences. This fellowship showed me the importance of being connected to different people, valuing different opinions and approaches.
So, to conclude, I would recommend everyone with a specific interest in genetic epilepsies to visit Filadelfia Epilepsy Center.
With thanks to Rikke, Guido, Elena and Allan for their excellent guidance, teaching and support!
Joana Dionísio, Lisbon, Portugal
Term of Fellowship: June – August 2023
Hosting department: Muscle and Myasthenia Service, King’s College Hospital, London, UK
Supervisor: Dr Fiona Norwood
My EAN Clinical Fellowship at the Muscle and Myasthenia Service of King’s College Hospital (KCH), London, started on 5 June 2023 and had a duration of 12 weeks. I had the incredible opportunity of being supervised by Dr Fiona Norwood, who is a Consultant Neurologist with a vast experience in neuromuscular disorders, and an Honorary Senior Lecturer with KCH. She is also the Lead for the Muscle and Myasthenia Service of KCH.
My main objectives for this educational stay were to improve my clinical skills in the evaluation of a neuromuscular patient, to understand the different neurophysiological studies in this area (namely nerve conduction studies, electromyography, and muscle biopsy), and to collaborate on scientific projects. I am happy to end this clinical fellowship knowing that these were fulfilled.
During my fellowship, I had the opportunity to attend different clinics and academic meetings and to observe neurophysiological studies.
At the Myasthenia Clinic, along with Dr Fiona Norwood and a Neuromuscular Fellow, Dr Swati Trivedi, I observed semi-autonomously several myasthenia patients (or those with a suspected neuromuscular junction disorder) and was able to discuss their symptoms and signs, their clinical evolution, and their treatment, especially regarding immunosuppression. I also observed several patients at the Programmed Investigation Unit, while they were having their intravenous infusions (e.g.: immunoglobulins), along with the Myasthenia Senior Nurse Specialist, Xia Zhang. This clinic allowed me to enhance my knowledge of myasthenia gravis and how to correctly manage both chronic myasthenic patients and patients with symptomatic aggravation. I was also very fortunate to attend the Congenital Myasthenia Clinic, which takes place periodically and is done along with colleagues from the University of Oxford.
At the Muscle Clinic, along with Dr Fiona Norwood and semi-autonomously, I saw several patients with a previously diagnosed neuromuscular condition or patients with a clinical suspicion. This clinic provided me with real insight into the many muscle conditions due to the diversity of clinical presentations. It was like watching a neuromuscular textbook coming to life. It also perfected my anamnesis and neurological examination when suspecting a muscle condition. At this clinic, I saw different types of muscle conditions, namely myotonic dystrophies, limb-girdle muscular dystrophies, fascioscapulohumeral muscular dystrophies, dysthrophinopathies, congenital muscular dystrophies, congenital myopathies, distal myopathies, metabolic myopathies, and inclusion body myositis. I also discussed the different strategies of genetic testing with the Deputy Genomic Practitioner, Dr Zoulikha Belblidia.
At the Motor Neuron Disorders Clinic, I took part in the weekly meeting, where patients’ needs were discussed with a multidisciplinary team in terms of palliative care, respiratory assessments, physiotherapy, occupational therapy, speech therapy and social care. At Dr Cathy Ellis’s clinic, I was able to assess patients with different presentations of motor neuron disease and participate in further discussions with them regarding their disease progression and their day-to-day life adaptations.
At the Myositis Clinic, I was able to observe several rheumatological patients with Dr Patrick Gordon. Most of these patients had an inflammatory condition in the muscle, but also other types of autoimmune manifestations. I saw patients with dermatomyositis, vasculitis, and connective tissue diseases. In this clinic, I had the chance to discuss the importance of several myositis-specific and myositis-associated antibodies when it comes to diagnosis and prognosis and to be more familiar with myositis-associated skin manifestations.
Parallel to these clinics, I also observed nerve conduction studies and electromyographies being performed by Dr Doreen Fialho. I gained more experience in interpreting their results and understanding the main technical difficulties that might influence an incorrect diagnosis. Furthermore, I also benefitted tremendously from observing specialist neurophysiotherapists Joanna Reffin and Francesca Morris evaluating neuromuscular patients from a physiotherapy point of view.
I also attended the weekly biopsy meeting, where muscle biopsies were presented, and their findings discussed. The neurology academic meeting was another weekly meeting that provided an interactive and educational approach to difficult clinical cases and topic reviews. I also had the opportunity to join the London Myology Forum Meeting.
I was very fortunate to be able to develop several investigation projects in the neuromuscular disorders field during my stay.
Regarding the practical aspects of my stay, although the EAN grant helped with the costs of my visit, its value was approximately €450 short of fully covering the costs, mostly due to accommodation expenses (around €1400 – 1600 per month). I used a rental platform called “Doctor in the House” to find secure accommodation within the KCH area.
Denmark Hill is well provided with transport – there are several bus options and a train station nearby. One can also easily find supermarkets and pharmacies in this area, especially when going towards Dulwich. Ruskin Park is right next to the hospital, and it is a lovely place to take a walk after work. As KCH is a part of King’s College Campus there are some options to work or study, namely the Weston Education Centre.
I would like to express my everlasting gratitude to Dr Fiona Norwood and all the KCH’s Muscle and Myasthenia Service, who so kindly took me in and ensured I had the best possible experience in clinical and academic terms. I would also like to thank the EAN for giving me the opportunity to broaden my horizons by granting me this Clinical Fellowship.