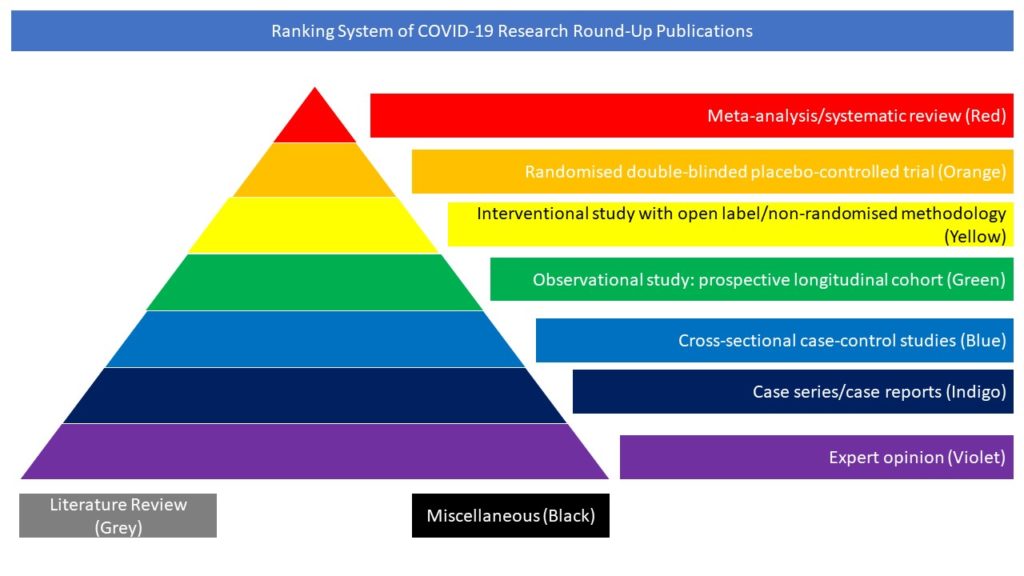
Cross-sectional case-control studies (Blue)
Read on for our pick of COVID-19-related cross-sectional case control studies from the scientific press for December 2022:
- Major neurological complications of COVID-19 comparative features and outcome
- Incidence of Epilepsy and Seizures Over the First 6 Months After a COVID-19 Diagnosis: A Retrospective Cohort Study
- Severe Neuro-COVID is associated with peripheral immune signatures, autoimmunity and neurodegeneration: a prospective cross-sectional study
Comparative features and outcomes of major neurological complications of COVID-19
The objective of this study was to assess neurological complications of SARS-CoV-2 infection and compare phenotypes and outcome in infected patients with and without selected neurological manifestations. The data source was represented by a registry established by the European Academy of Neurology during the first wave of COVID-19 pandemic. Neurologists collected data on patients with COVID-19 seen as in- and out-patients and in emergency rooms in 23 European and seven non-European countries. Prospective and retrospective data included patient’s demographics, lifestyle habits, comorbidities, main COVID-19 complications, hospital and ICU admissions, diagnostic tests, and outcome. Acute/subacute selected neurological manifestations in patients with COVID-19 were analysed comparing individuals with and without each condition for several risk factors. By July 31st 2021, 1523 patients (758 men, 756 women, and nine intersex/unknown, aged 16-101 years) were registered. Neurological manifestations were diagnosed in 1213 infected patients (79.6%). At study entry, 978 subjects (64.2%) had one or more chronic general and neurological comorbidities. Predominant acute/subacute neurological manifestations were cognitive dysfunction (N=449, 29.5%), stroke (N=392, 25.7%), sleep-wake disturbances (N=250, 16.4%), dysautonomia (N=224, 14.7%), peripheral neuropathy (N=145, 9.5%), movement disorders (N=142, 9.3%), ataxia (N=134, 8.8%), and seizures (N=126, 8.3%). These manifestations tended to differ with age, general and neurological comorbidities, infection severity and non-neurological manifestations, extent of association with other acute/subacute neurological manifestations, and outcome. The authors concluded that patients with COVID-19 and neurological manifestations present with distinct phenotypes. In particular, differences in age, general and neurological comorbidities, and infection severity characterize the various neurological manifestations of COVID-19.
Beghi E, Moro E, Davidescu EI, Popescu BO, Grosu O, Valzania F, Cotelli MS, Kiteva-Trenchevska G, Zakharova M, Kovács T, Armon C, Brola W, Yasuda CL, Maia LF, Lovrencic-Huzjan A, Laracho de Seabra MM, Avalos-Pavon R, Aamodt AH, Meoni S, Gryb V, Krehan I, Leone MA, Lolich M, Bianchi E, Rass V, Helbok R, Bassetti CLA; ENERGY Study Group. Major neurological complications of COVID-19 comparative features and outcome. Eur J Neurol. 2022 Oct 31. doi: 10.1111/ene.15617.
Incidence of Epilepsy and Seizures Over the First 6 Months After a COVID-19 Diagnosis: A Retrospective Cohort Study
The relationship between COVID-19 and epilepsy is uncertain. In this article the authors studied the potential association between COVID-19 and seizures or epilepsy in the six months after infection. They applied validated methods to an electronic health records network (TriNetX Analytics) of 81 million people and closely matched people with COVID-19 infections to those with influenza. In each cohort, the incidence and hazard ratios (HRs) of seizures and of epilepsy were measured. The authors stratified data by age and by whether the person was hospitalized during the acute infection and then explored time-varying HRs to assess temporal patterns of seizure or epilepsy diagnoses. 860,934 electronic health records were analyzed. After matching, this yielded two cohorts each of 152,754 patients. COVID-19 was associated with an increased risk of seizures and epilepsy compared to influenza. The incidence of seizures within 6 months of COVID-19 was 0.81% (95% CI, 0.75-0.88; HR compared to influenza 1.55 (1.39-1.74)). The incidence of epilepsy was 0.30% (0.26-0.34; HR compared to influenza 1.87 (1.54-2.28)). The HR of epilepsy after COVID-19 compared to influenza was greater in people who had not been hospitalized and in individuals aged under 16 years. The time of peak HR after infection differed by age and hospitalization status. The authors concluded that the incidence of new seizures or epilepsy diagnoses in the six months following COVID-19 was low overall, but higher than in matched patients with influenza. This difference was more marked in people who were not hospitalized, highlighting the risk of epilepsy and seizures even in those with less severe infection. Children appear at particular risk of seizures and epilepsy after COVID-19 providing another motivation to prevent COVID-19 infection in pediatric populations. That the varying time of peak risk related to hospitalization and age may provide clues as to the underlying mechanisms of COVID-associated seizures and epilepsy.
Taquet M, Devinsky O, Cross JH, Harrison PJ, Sen A. Incidence of Epilepsy and Seizures Over the First 6 Months After a COVID-19 Diagnosis: A Retrospective Cohort Study. Neurology. 2022 Nov 16:10.1212/WNL.0000000000201595. doi: 10.1212/WNL.0000000000201595.
Severe Neuro-COVID is associated with peripheral immune signatures, autoimmunity and neurodegeneration: a prospective cross-sectional study
Growing evidence links COVID-19 with acute and long-term neurological dysfunction. However, the pathophysiological mechanisms resulting in central nervous system involvement remain unclear, posing both diagnostic and therapeutic challenges. In this article the authors show outcomes of a cross-sectional clinical study (NCT04472013) including clinical and imaging data and corresponding multidimensional characterization of immune mediators in the cerebrospinal fluid (CSF) and plasma of patients belonging to different Neuro-COVID severity classes. The most prominent signs of severe Neuro-COVID were blood-brain barrier (BBB) impairment, elevated microglia activation markers and a polyclonal B cell response targeting self-antigens and non-self-antigens. COVID-19 patients showed decreased regional brain volumes associating with specific CSF parameters, however, COVID-19 patients characterized by plasma cytokine storm are presenting with a non-inflammatory CSF profile. Post-acute COVID-19 syndrome strongly associates with a distinctive set of CSF and plasma mediators. Collectively, the authors identify several potentially actionable targets to prevent or intervene with the neurological consequences of SARS-CoV-2 infection.
Etter MM, Martins TA, Kulsvehagen L, Pössnecker E, Duchemin W, Hogan S, Sanabria-Diaz G, Müller J, Chiappini A, Rychen J, Eberhard N, Guzman R, Mariani L, Melie-Garcia L, Keller E, Jelcic I, Pargger H, Siegemund M, Kuhle J, Oechtering J, Eich C, Tzankov A, Matter MS, Uzun S, Yaldizli Ö, Lieb JM, Psychogios MN, Leuzinger K, Hirsch HH, Granziera C, Pröbstel AK, Hutter G. Severe Neuro-COVID is associated with peripheral immune signatures, autoimmunity and neurodegeneration: a prospective cross-sectional study. Nat Commun. 2022 Nov 9;13(1):6777. doi: 10.1038/s41467-022-34068-0.