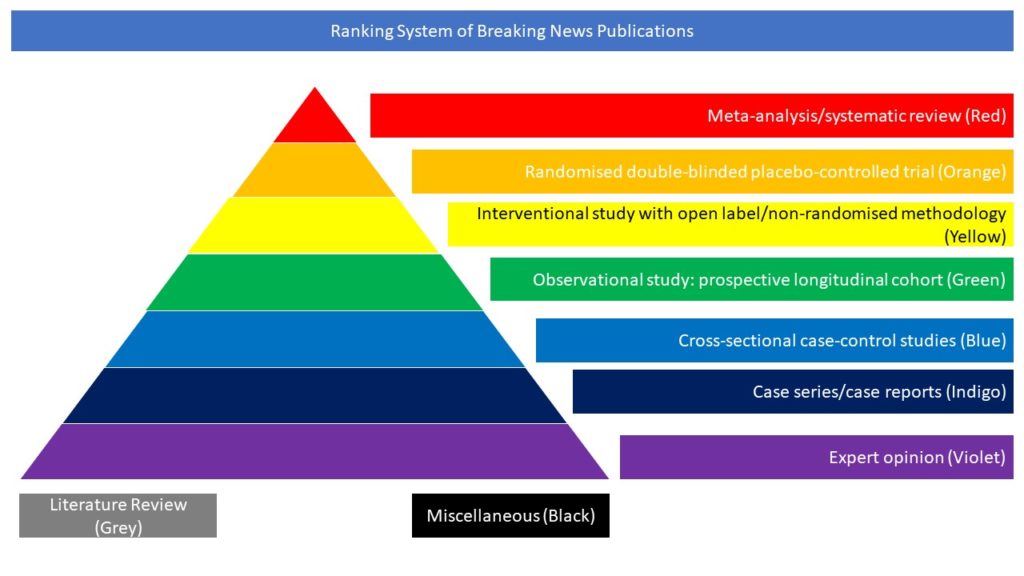
Cross-sectional case-control studies (Blue)
Read on for our highlighted selection of Covid-related cross-sectional case control studies from the scientific press for March 2022:
- COVID-19 and Risk of Acute Ischemic Stroke Among Medicare Beneficiaries Aged 65 Years or Older: Self-Controlled Case Series Study
- Altered motor cortex physiology and dysexecutive syndrome in patients with fatigue and cognitive difficulties after mild COVID-19
COVID-19 and Risk of Acute Ischemic Stroke Among Medicare Beneficiaries Aged 65 Years or Older: Self-Controlled Case Series Study
Findings of association between COVID-19 and stroke remain inconsistent, ranging from significant association, absence of association to less than expected ischemic stroke among hospitalized patients with COVID-19. The present study examined the association between COVID-19 and risk of acute ischemic stroke (AIS). The authors included 37,379 Medicare fee-for-service (FFS) beneficiaries aged ≥65 years diagnosed with COVID-19 from April 1, 2020 through February 28, 2021 and AIS hospitalization from January 1, 2019 through February 28, 2021. A self-controlled case series design was used to examine the association between COVID-19 and AIS and estimated the incident rate ratios (IRR) by comparing incidence of AIS in risk periods (0–3, 4–7, 8–14, 15–28 days after diagnosis of COVID-19) vs. control periods. Among 37,379 Medicare FFS beneficiaries with COVID-19 and AIS, the median age at diagnosis of COVID-19 was 80.4 (interquartile range 73.5–87.1) years and 56.7% were women. When AIS at day of exposure (day=0) included in the risk periods, IRRs at 0–3, 4–7, 8–14, and 15–28 days following COVID-19 diagnosis were 10.3 (95% confidence interval 9.86–10.8), 1.61 (1.44–1.80), 1.44 (1.32–1.57), and 1.09 (1.02–1.18); when AIS at day 0 excluded in the risk periods, the corresponding IRRs were 1.77 (1.57–2.01) (day 1-3), 1.60 (1.43–1.79), 1.43 (1.31–1.56), and 1.09 (1.01–1.17), respectively. The association appeared to be stronger among younger beneficiaries and among beneficiaries without prior history of stroke but largely consistent across sex and race/ethnicities. The risk of AIS among Medicare FFS beneficiaries was ten times (day 0 cases in the risk period) as high during the first 3 days after diagnosis of COVID-19 as during the control period and the risk associated with COVID-19 appeared to be stronger among those aged 65–74 years and those without prior history of stroke. The authors concluded that this study provides Class IV evidence that SARS-CoV-2 infection, the virus that causes COVID-19, is associated with increased risk of AIS in the first three days after diagnosis in Medicare FFS beneficiaries ≥ 65 years age.
Yang Q, Tong X, George MG, Chang A, Merritt RK. COVID-19 and Risk of Acute Ischemic Stroke Among Medicare Beneficiaries Aged 65 Years or Older: Self-Controlled Case Series Study. Neurology. 2022 Feb 3:10.1212/WNL.0000000000013184. doi: 10.1212/WNL.0000000000013184.
Altered motor cortex physiology and dysexecutive syndrome in patients with fatigue and cognitive difficulties after mild COVID-19
Fatigue and cognitive difficulties are reported as the most frequently persistent symptoms in patients after mild SARS-CoV-2 infection. In this article the authors performed an extensive neurophysiological and neuropsychological assessment of such patients focusing on motor cortex physiology and executive cognitive functions. 67 patients were enrolled complaining of fatigue and/or cognitive difficulties after resolution of mild SARS-CoV-2 infection and 22 healthy controls (HC). Persistent clinical symptoms were investigated by means of a 16-item questionnaire. Fatigue, exertion, cognitive difficulties, mood and “well-being” were evaluated through self-administered tools. Utilizing transcranial magnetic stimulation of the primary motor cortex (M1) the authors evaluated resting motor threshold (RMT), motor evoked potential (MEP) amplitude, cortical silent period (SP) duration, short-interval intracortical inhibition (SICI), intracortical facilitation (ICF), long-interval intracortical inhibition (LICI), and short-latency afferent inhibition (SAI). Global cognition and executive functions were assessed with screening tests. Attention was measured with computerized tasks. Post COVID-19 patients reported a mean of 4.9 persistent symptoms, high levels of fatigue, exertion, cognitive difficulties, low levels of well-being and depressive symptoms. Compared to HC, patients presented higher RMTs, lower MEP amplitudes and longer SPs, concurring with reduced M1 excitability. LICI and SAI were also impaired, indicating altered GABAB- and cholinergic neurotransmission. SICI and ICF were not affected. Patients also showed poorer global cognition and executive functions as compared to HC and a clear impairment in sustained and executive attention. The authors concluded that patients with fatigue and cognitive difficulties following mild COVID-19 present altered excitability and neurotransmission within M1 and deficits in executive functions and attention.
Ortelli P, Ferrazzoli D, Sebastianelli L, Maestri R, Dezi S, Spampinato D, Saltuari L, Alibardi A, Engl M, Kofler M, Quartarone A, Koch G, Oliviero A, Versace V. Altered motor cortex physiology and dysexecutive syndrome in patients with fatigue and cognitive difficulties after mild COVID-19. Eur J Neurol. 2022 Feb 9. doi: 10.1111/ene.15278.