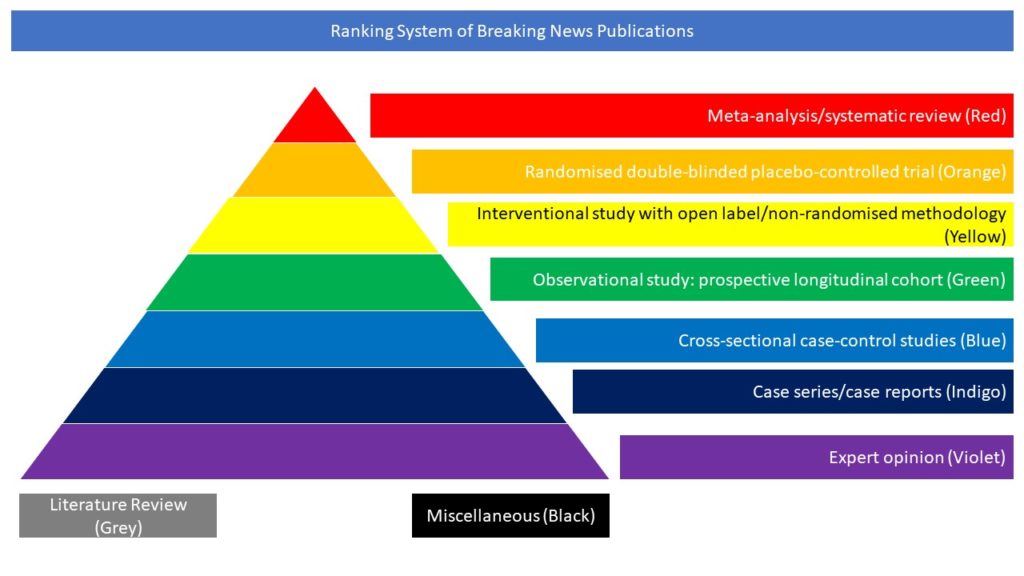
Case series/case reports (Indigo)
Read on for our highlighted selection of Covid-related case series and case reports from the scientific press for January 2022:
- Reduced neutralisation of SARS-CoV-2 omicron B.1.1.529 variant by post-immunisation serum
- COVID-19 Infection in Fingolimod- or Siponimod-Treated Patients – Case Series
- Motor and respiratory decline in patients with Late-onset Pompe disease after cessation of enzyme replacement therapy during COVID-19 pandemic
- COVID-19 Infection in Patients with Late-Onset Pompe Disease
- Headache Worsening after COVID-19 Vaccination: An Online Questionnaire-Based Study on 841 Patients with Migraine
- Post-vaccine COVID-19 in patients with multiple sclerosis or neuromyelitis optica
Reduced neutralisation of SARS-CoV-2 omicron B.1.1.529 variant by post-immunisation serum
At present, delta variant is estimated to have caused more than 99% of COVID-19 infections worldwide; however, a new variant of concern, omicron (B.1.1.529), was reported first in South Africa on Nov 24, 2021, but has since been reported in multiple countries. Early reports from South Africa suggest that omicron is highly transmissible, in a population where 60–80% already show serological evidence of previous infection or vaccination, suggesting that omicron is able to break through natural and vaccine-induced immunity; although early reports do not indicate more severe disease.
In this article the authors report the results of neutralisation assays using an isolate of omicron obtained from an infected case in the UK. Neutralisation assays were done on sera from individuals from the immunology cohort of the Com-COV2 study, who were seronegative at enrolment (defined by anti-nucleocapsid IgG). Participants were vaccinated with two doses of Oxford–AstraZeneca’s ChAdOx1 nCoV-19 (ChAd; n=22), or two doses of Pfizer–BioNTech’s BNT162b2 (BNT; n=21). Samples were obtained 28 days (range 25–32) following the second immunisation. The authors found a substantial decrease in neutralisation titre in recipients of both homologous ChAd and BNT primary courses, with evidence of some recipients not neutralising at all. This reduction in neutralisation titre will probably be more pronounced at later timepoints.
Dejnirattisai W, Shaw RH, Supasa P, Liu C, Stuart AS, Pollard AJ, Liu X, Lambe T, Crook D, Stuart DI, Mongkolsapaya J, Nguyen-Van-Tam JS, Snape MD, Screaton GR; Com-COV2 study group. Reduced neutralisation of SARS-CoV-2 omicron B.1.1.529 variant by post-immunisation serum. Lancet. 2021 Dec 20:S0140-6736(21)02844-0. doi: 10.1016/S0140-6736(21)02844-0.
COVID-19 Infection in Fingolimod- or Siponimod-Treated Patients – Case Series
The objective of this study was to descriptive analysis of COVID-19 infection in patients with multiple sclerosis (MS) receiving fingolimod or siponimod. The authors reviewed the cases of COVID-19 from postmarketing or ongoing clinical trials reported to Novartis through December 27, 2020. As of December 27, 2020, 283 cases had been reported in fingolimod-treated patients. The mean age was 44 years (from n = 224; range 11–69 years), and 190 were women. Of 161 cases with available information, 138 were asymptomatic (6), mild (100), or moderate (32); 50 cases required hospitalization. At the last follow-up, 140 patients were reported as recovered/recovering, condition was unchanged in 22, and deteriorated in 3 patients; 4 patients had a fatal outcome. Information was not available for 114 patients. Of the 54 cases of COVID-19 reported in siponimod-treated patients, 45 were from the postmarketing setting and 9 from an ongoing open-label clinical trial. The mean age was 54 years (from n = 45; range 31–70), and 30 were women. Of 28 cases with available information, 24 were asymptomatic (2), mild (17), or moderate (5); 9 cases required hospitalization. At the last follow-up, 27 patients were reported as recovered/recovering, condition remained unchanged for 1, and 3 patients had a fatal outcome. Information was not available for 23 patients. Based on a review of available information, the risk of more severe COVID-19 in patients receiving fingolimod or siponimod seems to be similar to that reported in the general population and the MS population with COVID-19. However, limitations of spontaneous reporting, especially missing data, should be considered in the interpretation of these observations.
Sullivan R, Kilaru A, Hemmer B, Campbell Cree BA, Greenberg BM, Kundu U, Hach T, DeLasHeras V, Ward BJ, Berger J. COVID-19 Infection in Fingolimod- or Siponimod-Treated Patients: Case Series. Neurol Neuroimmunol Neuroinflamm. 2021 Nov 30;9(1):e1092. doi: 10.1212/NXI.0000000000001092.
Motor and respiratory decline in patients with Late-onset Pompe disease after cessation of enzyme replacement therapy during COVID-19 pandemic
Data on interruption of enzyme replacement therapy are scarce in late-onset Pompe disease. Due to the COVID-19 crisis, 8 neuromuscular reference centers in France were obligated to stop the treatment for 31 patients. In this article the authors collected the motor and respiratory data from the French registry, before COVID-19 and at treatment restart. In 2.2 months (mean), patients showed a significant deterioration of 37 meters (mean) in the 6-minute walk test and a loss of 210 mL (mean) of forced vital capacity, without ad integrum restoration after 3 months of ERT restart. The authors concluded that this national study based on data from the French Pompe registry shows that the interruption of enzyme replacement therapy, even as short as only few months, worsens Pompe patients’ motor and respiratory function.
Tard C, Salort-Campana E, Michaud M, Spinazzi M, Nadaj Pakleza A, Durr H, Bouhour F, Lefeuvre C, Thomas R, Arrassi A, Taouagh N; Pompe study group, Solé G, Laforêt P. Motor and respiratory decline in patients with Late-onset Pompe disease after cessation of enzyme replacement therapy during COVID-19 pandemic. Eur J Neurol. 2021 Dec 20. doi: 10.1111/ene.15222.
COVID-19 Infection in Patients with Late-Onset Pompe Disease
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2/COVID-19) is frequently more severe in individuals with preexisting respiratory and cardiovascular conditions The impact on patients with neuromuscular disorders is concerning, but largely unknown. Late-onset Pompe disease (LOPD), is a lysosomal storage disorder characterized by progressive skeletal and respiratory muscle degeneration. Mortality is typically caused by respiratory failure. In this case series the authors examined the impact of COVID-19 in 4 patients with LOPD. All patients experienced a mild/moderate illness from COVID-19 and did not require hospitalization. Neurological worsening occurred in one; with no change in physical ability in the other three, and respiratory symptoms remained stable in all four. The authors concluded that COVID-19 infection can result in a benign course in some patients with LOPD. However, individuals with LOPD remain at high risk and should receive COVID-19 vaccinations and exercise precautions to avoid exposure to COVID-19 infection.
Avelar J, Wencel M, Chumakova A, Mozaffar T. COVID-19 Infection in Patients with Late-Onset Pompe Disease. Muscle Nerve. 2021 Dec 24. Doi: 10.1002/mus.27482.
Headache Worsening after COVID-19 Vaccination: An Online Questionnaire-Based Study on 841 Patients with Migraine
Vaccines have represented the breakthrough in the fight against COVID-19. Based on reported headache attacks after vaccination in randomized controlled trials, the authors of this article focused on the effects of COVID-19 vaccine administration on the migraine population, using an online questionnaire published on Italian Facebook groups oriented to headache patients. They collected data about the demographics and clinical parameters of migraine severity, COVID-19 infection, vaccination, and characteristics of headaches following vaccination. Out of 841 migraine patients filling in the questionnaire, 66.47% and 60.15% patients experienced a headache attack (from 1 hour to 7 days) after the first and the second vaccine dose, respectively. The main finding concerns headaches perceived by 57.60% of patients: attacks following vaccination were referred to as more severe (50.62% of patients), long-lasting (52.80% of patients) and hardwearing (49.69% of patients) compared to the usually experienced migraine attacks. This could be related to the production of inflammatory mediators such as type Iβ interferon. Considering the high prevalence of migraine in the general population, awareness of the possibility of headaches worsening following COVID-19 vaccination in these patients may allow both patients and clinicians to face this clinical entity with conscious serenity, and to reduce the waste of resources towards inappropriate health-care.
Silvestro M, Tessitore A, Orologio I, Sozio P, Napolitano G, Siciliano M, Tedeschi G, Russo A. Headache Worsening after COVID-19 Vaccination: An Online Questionnaire-Based Study on 841 Patients with Migraine. J Clin Med. 2021 Dec 16;10(24):5914. doi: 10.3390/jcm10245914.
Post-vaccine COVID-19 in patients with multiple sclerosis or neuromyelitis optica
Recent studies suggested that anti-CD20 and fingolimod may be associated with lower anti-spike protein-based immunoglobulin-G response following COVID-19 vaccination. In this article the authors evaluated if COVID-19 occurred despite vaccination among patients with multiple sclerosis (MS) and neuromyelitis optica (NMO), using the COVISEP registry. They report 18 cases of COVID-19 after two doses of BNT162b2-vaccination, 13 of which treated with anti-CD20 and four with fingolimod. COVID-19 severity was mild. The authors concluded that these results reinforce the recommendation for a third COVID-19 vaccine dose among anti-CD20 treated patients and stress the need for a prospective clinical and biological study on COVID-19 vaccine efficacy among MS and NMO patients.
Januel E, De Seze J, Vermersch P, Maillart E, Bourre B, Pique J, Moisset X, Bensa C, Maarouf A, Pelletier J, Vukusic S, Audoin B, Louapre C. Post-vaccine COVID-19 in patients with multiple sclerosis or neuromyelitis optica. Mult Scler. 2021 Dec 21:13524585211049737. doi: 10.1177/13524585211049737.