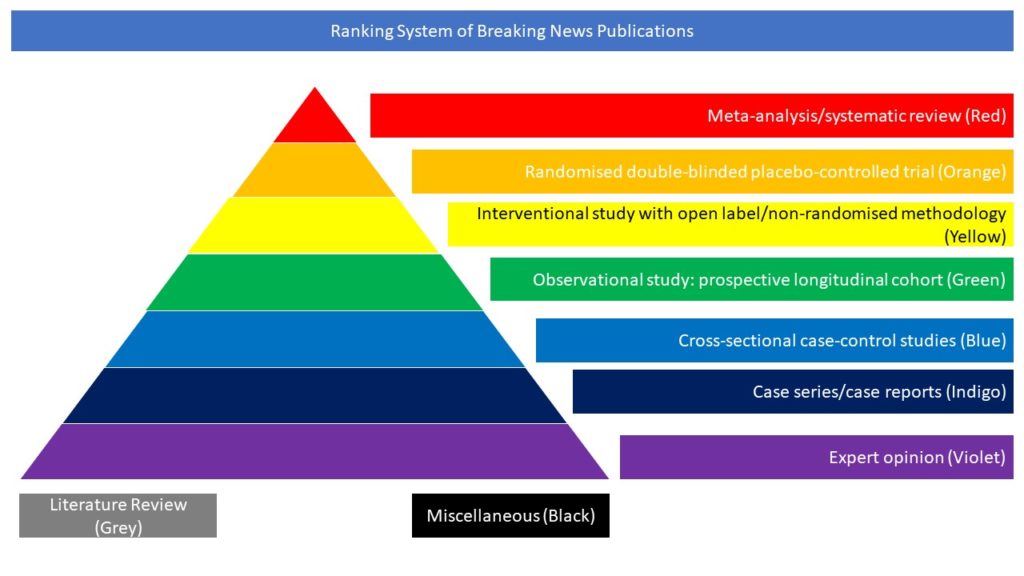
Case series/case reports (Indigo)
People with multiple sclerosis (MS) are a vulnerable group for severe COVID-19, particularly those taking immunosuppressive disease-modifying therapies (DMTs). In this article the authors examined the characteristics of COVID-19 severity in an international sample of people with MS. Data from 12 data-sources in 28 countries were aggregated (sources could include patients from 1-12 countries). Demographic (age, sex), clinical (MS-phenotype, disability), and DMT (untreated, alemtuzumab, cladribine, dimethyl-fumarate, glatiramer acetate, interferon, natalizumab, ocrelizumab, rituximab, siponimod, other DMTs) covariates were queried, alongside COVID-19 severity outcomes, hospitalisation, ICU admission, requiring artificial ventilation, and death. Characteristics of outcomes were assessed in patients with suspected/confirmed COVID-19 using multilevel mixed-effects logistic regression, adjusted for age, sex, MS-phenotype, and EDSS. 657(28.1%) with suspected and 1,683 (61.9%) with confirmed COVID-19 were analysed. Among suspected+confirmed and confirmed-only COVID-19, 20.9% and 26.9% were hospitalised, 5.4% and 7.2% were admitted to ICU, 4.1% and 5.4% required artificial ventilation, and 3.2% and 3.9% died. Older age, progressive MS-phenotype, and higher disability were associated with worse COVID-19 outcomes. Compared to dimethyl-fumarate, ocrelizumab and rituximab were associated with hospitalisation (aOR=1.56,95%CI=1.01- 2.41; aOR=2.43, 95%CI=1.48-4.02) and ICU admission (aOR=2.30,95%CI=0.98-5.39; aOR=3.93, 95%CI=1.56-9.89), though only rituximab was associated with higher risk of artificial ventilation (aOR=4.00, 95%CI=1.54-10.39). Compared to pooled other DMTs, ocrelizumab and rituximab were associated with hospitalisation (aOR=1.75,95%CI=1.29- 2.38; aOR=2.76,95%CI=1.87-4.07) and ICU admission (aOR=2.55,95%CI=1.49-4.36; aOR=4.32, 95%CI=2.27-8.23) but only rituximab with artificial ventilation (aOR=6.15,95%CI=3.09-12.27). Compared to natalizumab, ocrelizumab and rituximab were associated with hospitalisation (aOR=1.86,95%CI=1.13-3.07; aOR=2.88,95%CI=1.68-4.92) and ICU admission (aOR=2.13,95%CI=0.85-5.35; aOR=3.23,95%CI=1.17-8.91), but only rituximab with ventilation (aOR=5.52,95%CI=1.71-17.84). Importantly, associations persisted on restriction to confirmed COVID-19 cases. No associations were observed between DMTs and death. Stratification by age, MS-phenotype, and EDSS found no indications that DMT associations with COVID-19 severity reflected differential DMT allocation by underlying COVID-19 severity. Using the largest cohort of people with MS and COVID-19 available the authors demonstrated a consistent associations of rituximab with increased risk of hospitalization, ICU admission, and requiring artificial ventilation, and ocrelizumab with hospitalisation and ICU admission. Despite the study’s cross-sectional design, the internal and external consistency of these results with prior studies suggests rituximab/ocrelizumab use may be a risk factor for more severe COVID-19.
Associations of Disease-Modifying Therapies With COVID-19 Severity in Multiple Sclerosis
Steve Simpson-Yap, Edward De Brouwer, Tomas Kalincik, Nick Rijke, Jan A Hillert, Clare Walton, Gilles Edan, Yves Moreau, Tim Spelman, Lotte Geys, Tina Parciak, Clement Gautrais, Nikola Lazovski, Ashkan Pirmani, Amin Ardeshirdavanai, Lars Forsberg, Anna Glaser, Robert McBurney, Hollie Schmidt, Arnfin B Bergmann, Stefan Braune, Alexander Stahmann, Rodden Middleton, Amber Salter, Robert J. Fox, Anneke van der Walt, Helmut Butzkueven, Raed Alroughani, Serkan Ozakbas, Juan I Rojas, Ingrid van der Mei, Nupur Nag, Rumen Ivanov, Guilherme Sciascia do Olival, Alice Estavo Dias, Melinda Magyari, Doralina Brum, Maria Fernanda Mendes, Ricardo N Alonso, Richard S Nicholas, Johana Bauer, Aníbal Sebastián Chertcoff, Anna Zabalza, Georgina Arrambide, Alex Fidao, Giancarlo Comi, Liesbet Peeters. Neurology Oct 2021, 10.1212/WNL.0000000000012753; DOI: 10.1212/WNL.0000000000012753.