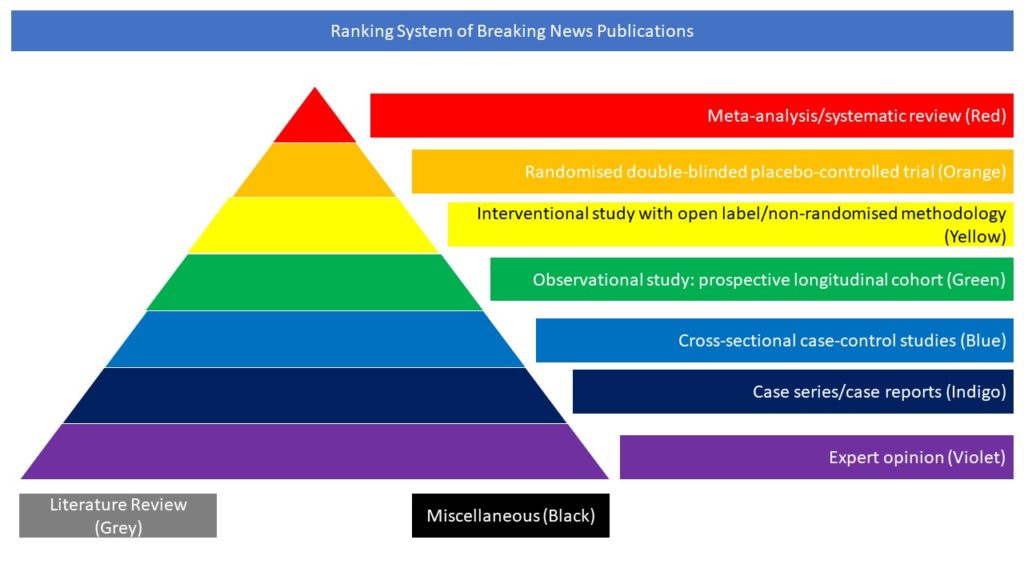
Cross-sectional case-control studies (Blue)
COVID-19 outcomes in patients with neurodegenerative disorders are not well understood, and the authors hypothesize there may be increased morbidity and mortality in this group. This retrospective cohort study was performed at three hospitals in the Chicagoland area. All patients hospitalized with COVID-19 infection with neurodegenerative disorder (ND) during a 3-month period (March 15-June 15, 2020) were included and compared with age-matched controls (CL) at 1:1 ratio. Primary outcomes were death, ICU admission and invasive ventilation. Secondary outcomes included presenting COVID-19 symptoms, development of encephalopathy, supplementary oxygen use, discharge disposition, and risk factors for mortality. The study included 132 neurodegenerative patients and 132 age-matched controls. 90-day mortality (ND 19.7% vs CL 23.5%, p=0.45) and ICU admission (ND 31.5% vs CL 35.9%, p=0.43) rates were not significantly different between the two groups. ND patients had lower rate of invasive ventilation (ND 11.4% vs CL 23.2%, p=0.0075) and supplementary oxygen use (ND 83.2% vs CL 95.1%, p=0.0012). ND patients were also more likely to have “altered mental status or confusion” as their presenting COVID-19 symptom, and less likely to present with respiratory symptoms. ND patients were discharged to nursing home or hospice at higher rates compared to CL.
The authors concluded that there was no difference in short-term mortality of ND patients hospitalized for COVID-19 compared to controls, but they may have higher rates of neurologic complications and disability. Future studies should address long-term outcomes.
Roshni Abee Patel, Glenn T. Stebbins, Ekta B. Kishen, Brandon Barton. COVID-19 Outcomes in Hospitalized Patients With Neurodegenerative Disease: A Retrospective Cohort Study. Neurol Clin Pract Jul 2021, 10.1212/CPJ.0000000000001117; DOI: 10.1212/CPJ.0000000000001117.