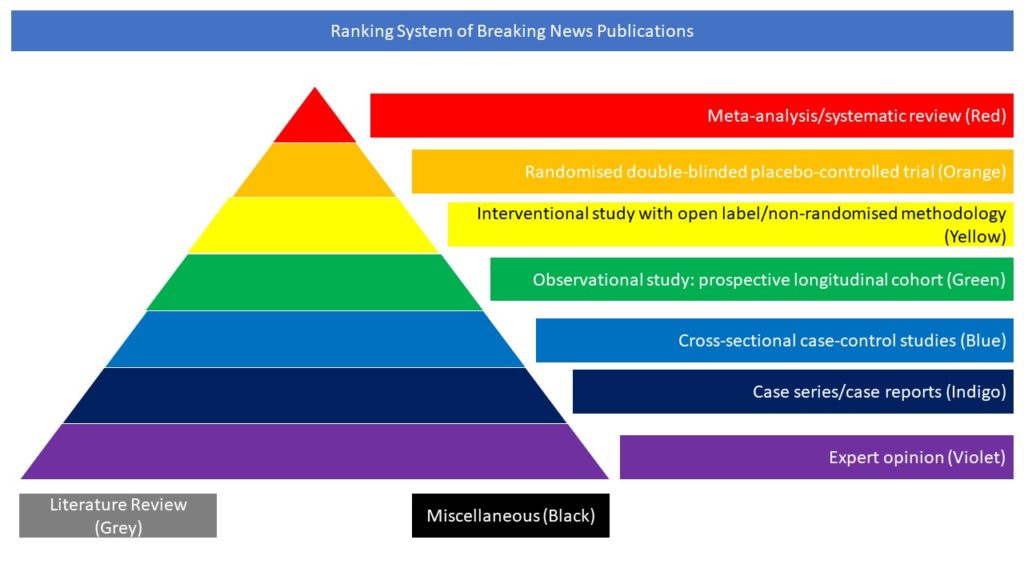
Cross-sectional case-control studies (Blue)
By Dementia and cognitive disorders
Author: Duan K.
This case-control study enrolled 58 COVID-19 positive and 62 COVID-19 negative patients, matched for age, gender and neurological admission causes, including brain tumors, encephalopathy, headache, epilepsy, stroke, transient ischemic attack, subarachnoid hemorrhage and peripheral nerves diseases. A multivariate approach, i.e., source-based morphometry (SBM), which uses independent component analysis (ICA) for data clustering, and traditional voxel-based morphometry (VBM) were applied. Cerebrovascular events, diabetes, hypertension and scanner site were included as covariates, and COVID-19 diagnosis was regressed out from the associations between grey matter volumes (GMV) independent components (IC) and clinical variables. COVID-19 positive patients had higher modified Rankin Scale (mRS) scores at discharge and worse outcomes. Lower GMV in the superior, medial, middle frontal gyri (first independent component (IC1)) was significantly associated with higher mRS scores, at discharge and after 6 months, to receiving oxygen therapy, and to higher psychomotor agitation. Febrile patients had lower GMV in inferior/middle temporal gyri and fusiform gyrus (IC2). The association between IC1 and oxygen therapy and fever and IC2 remained significant even in a subsample of 66 subjects with normal CT. No difference in GMV between COVID-19 positive and negative patients was found. The authors argue that COVID-19 affects fronto-temporal networks through hypoxia or fever.