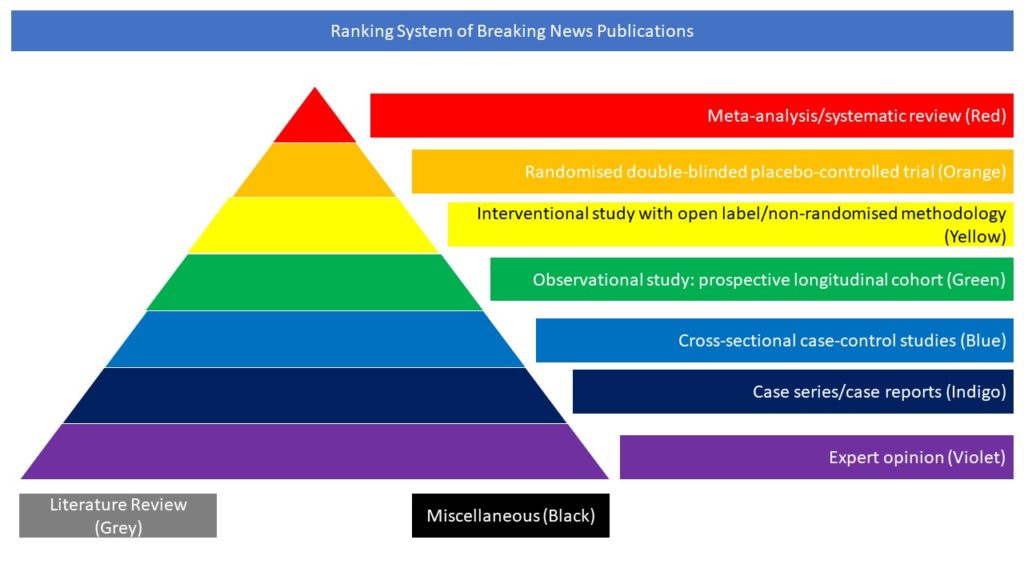
Miscellaneous (Black)
Breaking News by Cognitive disorders and Dementia Panel
This retrospective cohort study used the TriNetX electronic health records network, which has over 81 million patients’ data, to estimate the incidence of 14 neurological and psychiatric outcomes 6 months after COVID-19 infection. These included hemorrhagic and ischaemic stroke, parkinsonism, Guillain-Barré syndrome, nerve, nerve root and plexus disorders, myoneural junction and muscle disease, encephalitis, dementia, psychotic, mood and anxiety disorders, substance use and insomnia. The authors compared the incidence among 236,379 COVID-19 patients to two matched control groups of patients with either a diagnosis of influenza or other respiratory tract infections and to an additional four control groups with no respiratory infections. In COVID-19 patients the overall incidence of a neurological or psychiatric diagnosis was 33.62%, which was higher in patients admitted to ITU (46.42%) and patients with encephalopathy (62.34%). Overall neurological and psychiatric diagnoses were more prevalent in COVID-19 patients than in those who had influenza (hazard ratio (HR) 1.44), and those who had other respiratory tract infections (HR 1.16). The incidence of ischaemic stroke was 2.10%, rising to 9.35% in patients with encephalopathy. Dementia incidence in COVID-19 patients was 0.67%, increasing to 4.72% in patients with encephalopathy. Incidence of psychotic, mood and anxiety (23.98%) disorders was also high.
Taquet M; doi: 10.1016/S2215-0366(21)00084-5