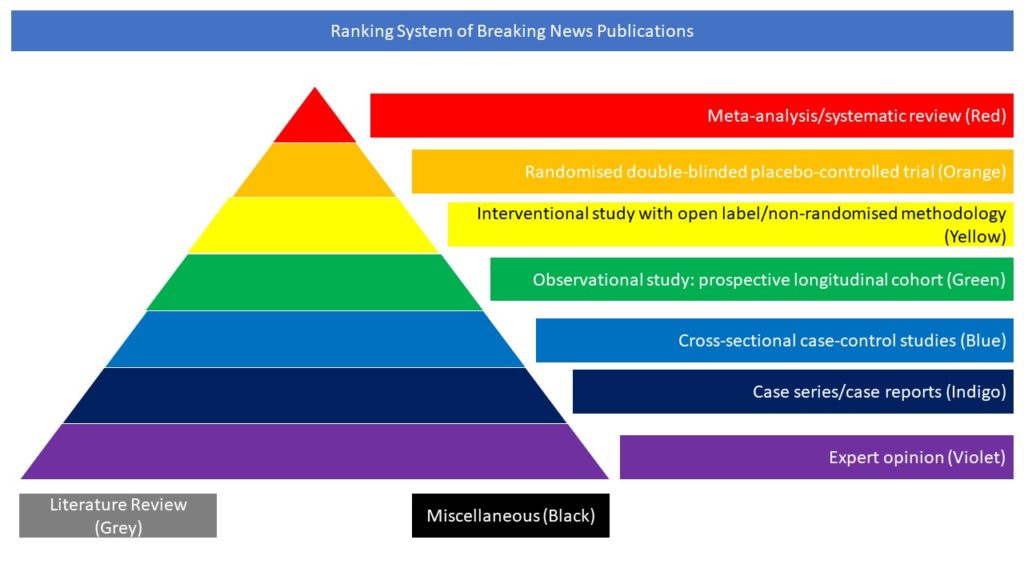
Observational study: prospective longitudinal cohort (Green)
Neurological complications of SARS‐CoV‐2 infection are noticed among critically‐ill patients soon after disease onset. Information on delayed neurological sequelae of SARS‐CoV‐2 infection is lacking. Following a longitudinal study design, the authors assessed the occurrence of cognitive decline among individuals with a history of mild symptomatic SARS‐CoV‐2 infection. Stroke‐ and seizure‐free Atahualpa residents aged ≥40 years who had pre‐pandemic cognitive assessments as well as normal brain MRI and EEG recordings, underwent repeated evaluations six months after a SARS‐CoV‐2 outbreak infection in Atahualpa. Patients requiring oxygen therapy, hospitalisation, and those who had initial neurological manifestations were excluded. Cognitive decline was defined as a reduction in Montreal Cognitive Assessment (MoCA) score between the post‐pandemic and pre‐pandemic assessments that was ≥4 points than the reduction observed between two pre‐pandemic MoCAs. The relationship between SARS‐CoV‐2 infection and cognitive decline was assessed by fitting logistic mixed models for longitudinal data as well as exposure‐effect models. Of 93 included individuals (mean age: 62.6±11 years), 52 (56%) had a history of mild symptomatic SARS‐CoV‐2 infection. Post‐pandemic MoCA decay was worse in seropositive individuals. Cognitive decline was recognised in 11/52 (21%) seropositive and 1/41 (2%) seronegative individuals. In multivariate analyses, the odds for developing cognitive decline were 18.1 times higher among SARS‐CoV‐2 seropositive individuals (95% C.I.: 1.75 – 188; p=0.015). Exposure‐effects models confirmed this association (β: 0.24; 95% C.I.: 0.07 – 0.41; p=0.006). The authors concluded that this study provides evidence of cognitive decline among individuals with mild symptomatic SARS‐CoV‐2 infection. The pathogenesis of this complication remains unknown.