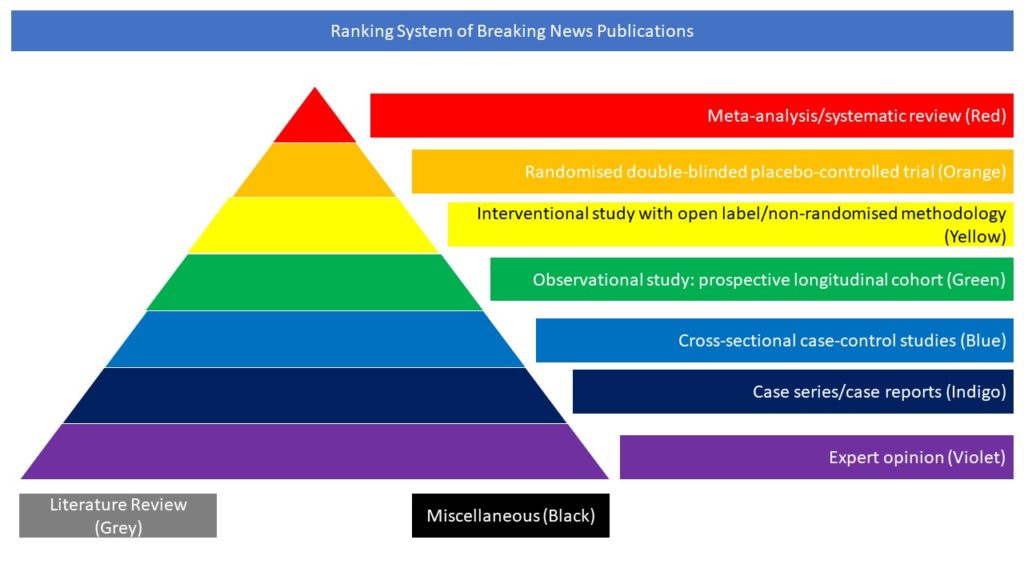
Interventional study with open label/non-randomised methodology (Yellow)
Patients with COVID-19 pneumonia have an excess of inflammation and increased concentrations of cytokines including interleukin-1 (IL-1). In this article, the authors aimed to determine whether anakinra, a recombinant human IL-1 receptor antagonist, could improve outcomes in patients in hospital with mild-to-moderate COVID-19 pneumonia. In this multicentre, open-label, Bayesian randomised clinical trial (CORIMUNO-ANA-1), nested within the CORIMUNO-19 cohort, the authors enrolled patients from 16 University hospitals in France with mild-to-moderate COVID-19 pneumonia, severe acute respiratory syndrome coronavirus 2 infection confirmed by real-time RT-PCR, requiring at least 3 L/min of oxygen by mask or nasal cannula but without ventilation assistance, a score of 5 on the WHO Clinical Progression Scale (WHO-CPS), and a C-reactive protein serum concentration of more than 25 mg/L not requiring admission to the intensive care unit at admission to hospital. Eligible patients were randomly assigned (1:1) using a web-based secure centralised system, stratified by centre and blocked with varying block sizes (randomly of size two or four), to either usual care plus anakinra (200 mg twice a day on days 1–3, 100 mg twice on day 4, 100 mg once on day 5) or usual care alone. Usual care was provided at the discretion of the site clinicians. The two co-primary outcomes were the proportion of patients who had died or needed non-invasive or mechanical ventilation by day 4 (ie, a score of >5 on the WHO-CPS) and survival without need for mechanical or non-invasive ventilation (including high-flow oxygen) at day 14. All analyses were done on an intention-to-treat basis. Between April 8 and April 26, 2020, 153 patients were screened. The study was stopped early following the recommendation of the data and safety monitoring board, after the recruitment of 116 patients: 59 were assigned to the anakinra group, and 57 were assigned to the usual care group. Two patients in the usual care group withdrew consent and were not analysed. In the analysable population, the median age was 66 years (IQR 59 to 76) and 80 (70%) participants were men. In the anakinra group, 21 (36%) of 59 patients had a WHO-CPS score of more than 5 at day 4 versus 21 (38%) of 55 in the usual care group (median posterior absolute risk difference [ARD] −2·5%, 90% credible interval [CrI] −17·1 to 12·0), with a posterior probability of ARD of less than 0 (ie, anakinra better than usual care) of 61·2%. At day 14, 28 (47%; 95% CI 33 to 59) patients in the anakinra group and 28 (51%; 95% CI 36 to 62) in the usual care group needed ventilation or died, with a posterior probability of any efficacy of anakinra (hazard ratio [HR] being less than 1) of 54·5% (median posterior HR 0·97; 90% CrI 0·62 to 1·52). At day 90, 16 (27%) patients in the anakinra group and 15 (27%) in the usual care group had died. Serious adverse events occurred in 27 (46%) patients in the anakinra group and 21 (38%) in the usual care group (p=0·45).
The authors concluded that anakinra did not improve outcomes in patients with mild-to-moderate COVID-19 pneumonia. However, further studies are needed to assess the efficacy of anakinra in other selected groups of patients with more severe COVID-19.