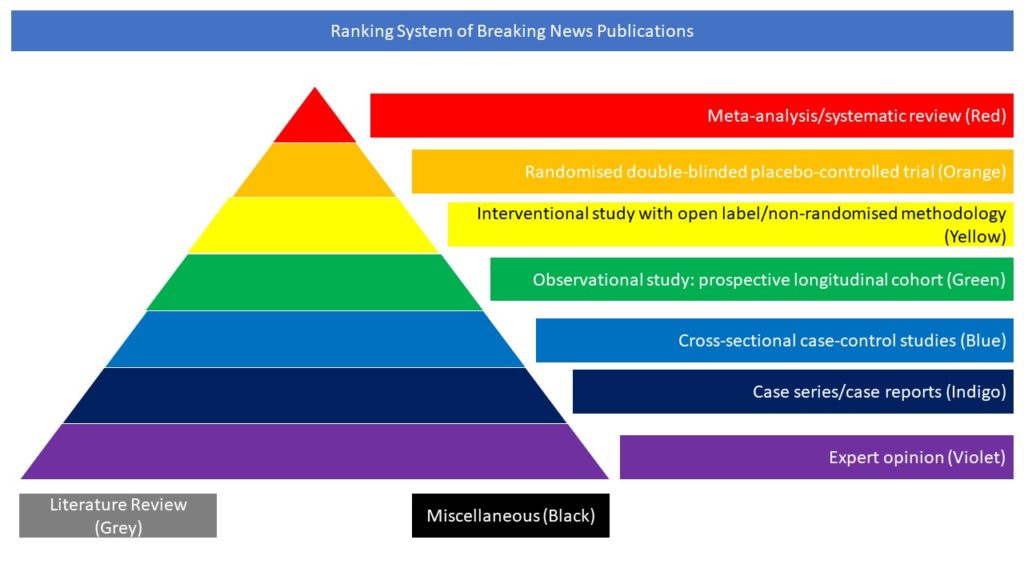
Interventional study with open label/non-randomised methodology (Yellow)
Efficacious vaccines are urgently needed to contain the ongoing COVID-19 pandemic. A candidate vaccine, Ad26.COV2.S, is a recombinant, replication-incompetent adenovirus serotype 26 (Ad26) vector encoding a full-length and stabilised SARS-CoV-2 spike protein.
In this multicentre, placebo-controlled, phase 1–2a trial, the authors randomly assigned healthy adults between the ages of 18 and 55 years (cohort 1) and those 65 years of age or older (cohort 3) to receive the Ad26.COV2.S vaccine at a dose of 5×1010 viral particles (low dose) or 1×1011 viral particles (high dose) per millilitre or placebo in a single-dose or two-dose schedule. Longer-term data comparing a single-dose regimen with a two-dose regimen are being collected in cohort 2; those results are not reported in this article. The primary endpoints were the safety and reactogenicity of each dose schedule. After the administration of the first vaccine dose in 805 participants in cohorts 1 and 3 and after the second dose in cohort 1, the most frequent solicited adverse events were fatigue, headache, myalgia, and injection-site pain. The most frequent systemic adverse event was fever. Systemic adverse events were less common in cohort 3 than in cohort 1 and in those who received the low vaccine dose than in those who received the high dose.
Reactogenicity was lower after the second dose. Neutralising-antibody titres against wild-type virus were detected in 90% or more of all participants on day 29 after the first vaccine dose (geometric mean titer [GMT], 224 to 354) and reached 100% by day 57 with a further increase in titres (GMT, 288 to 488), regardless of vaccine dose or age group. Titres remained stable until at least day 71. A second dose provided an increase in the titre by a factor of 2.6 to 2.9 (GMT, 827 to 1266). Spike-binding antibody responses were similar to neutralising-antibody responses. On day 14, CD4+ T-cell responses were detected in 76 to 83% of the participants in cohort 1 and in 60 to 67% of those in cohort 3, with a clear skewing toward type 1 helper T cells. CD8+ T-cell responses were robust overall but lower in cohort 3. The authors concluded that the safety and immunogenicity profiles of Ad26.COV2.S support further development of this vaccine candidate.