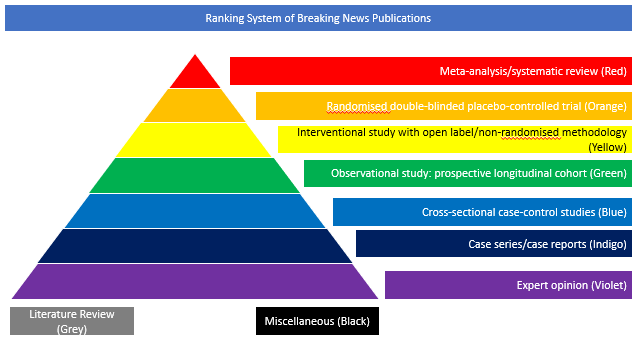
Observational study: prospective longitudinal cohort (Green)
The aim of this multicentre, European, cohort study involving 34 stroke centres in France, Italy, Spain, and Belgium, was to study early outcomes after mechanical thrombectomy (MT) in patients with COVID-19. Data were collected between March 1, 2020 and May 5, 2020. Consecutive laboratory-confirmed COVID-19 cases with large vessel occlusion, who were treated with MT, were included. The primary investigated outcome was the 30-day mortality while secondary outcomes included: early neurological improvement (National Institutes of Health Stroke Scale improvement ≥8 points or 24 hours National Institutes of Health Stroke Scale 0-1), successful reperfusion (modified Thrombolysis in Cerebral Infarction grade ≥2b), and symptomatic intracranial haemorrhage. The authors evaluated 93 patients with COVID-19 with large vessel occlusion who underwent MT (median age, 71 years [interquartile range, 59-79]; 63 men [67.7%]). Median pretreatment National Institutes of Health Stroke Scale and Alberta Stroke Program Early Computed Tomography score were 17 (interquartile range, 11-21) and 8 (interquartile range, 7-9), respectively. Anterior circulation acute ischemic stroke represented 93.5% of cases. The rate of modified Thrombolysis in Cerebral Infarction scores 2b to 3 was 79.6% (74 patients [95% CI, 71.3-87.8]). Thirty-day mortality was 29% (27 patients [95% CI, 20-39.4]). Early neurological improvement was seen in 19.5% (17 patients [95% CI, 11.8-29.5]), and symptomatic intracranial hemorrhage was seen in 5.4% (5 patients [95% CI, 1.7-12.1]). Patients who died at 30 days exhibited significantly lower lymphocyte count, higher levels of aspartate, and LDH (lactate dehydrogenase). After adjustment for age, initial National Institutes of Health Stroke Scale, Alberta Stroke Program Early Computed Tomography score, and successful reperfusion, these biological markers remained associated with increased odds of 30-day mortality (adjusted odds ratio of 2.70 [95% CI, 1.21-5.98] per SD-log decrease in lymphocyte count, 2.66 [95% CI, 1.22-5.77] per SD-log increase in aspartate, and 4.30 [95% CI, 1.43-12.91] per SD-log increase in LDH). The authors concluded that the 29% rate of 30-day mortality after MT among patients with COVID-19 is not negligible. Abnormalities of lymphocyte count, LDH and aspartate may depict patient’s profiles with poorer outcomes after MT.
DOI: 10.1161/STROKEAHA.120.031514