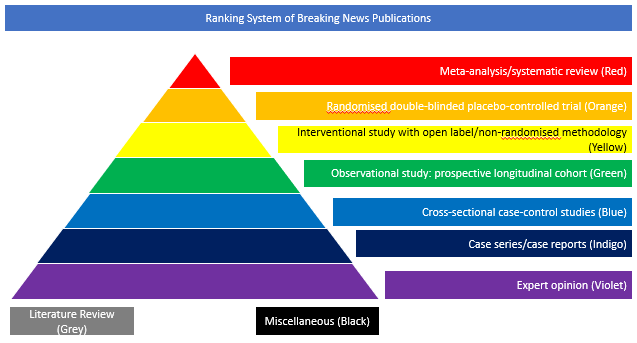
Case series/case reports (Indigo)
In this paper, the authors aimed to assess risk factors associated with intracerebral haemorrhage (ICH) in COVID-19 patients. The authors performed a retrospective cohort study of adult patients admitted to NYU Langone Health system between March 1 and April 27 2020. Inclusion criteria were a positive nasopharyngeal swab polymerase chain reaction test result and presence of primary non-traumatic intracranial hemorrhage or haemorrhagic conversion of ischaemic stroke on neuroimaging. Patients with intracranial procedures, malignancy, or vascular malformations were excluded. The authors used regression models to estimate odds ratios and 95% confidence intervals (OR, 95% CI) of the association between ICH and a number of covariates. Moreover, they applied regression models to determine associations between ICH and mortality. Among 3824 patients admitted with COVID-19, 755 patients had neuroimaging and 416 patients were identified after exclusion criteria were applied. The mean (standard deviation) age was 69.3 years (16.2), 35.8% were women, and 34.9% were receiving therapeutic anticoagulation. ICH occurred in 33 (7.9%) patients. Older age, non-Caucasian race, respiratory failure requiring mechanical ventilation, and therapeutic anticoagulation were associated with an increased risk of ICH on univariate analysis (p < 0.01 for each variable). In adjusted regression models, anticoagulation usage was associated with a five-fold increased risk of ICH (OR 5.26, 95% CI 2.33–12.24, p < 0.001). ICH was associated with increased mortality (adjusted OR 2.6, 95 % CI 1.2–5.9). The authors concluded that anticoagulation usage is associated with increased risk of ICH in patients with COVID-19. Moreover, they underline that further investigation is required to elucidate underlying mechanisms and prevention strategies in this population.
DOI: https://doi.org/10.1007/s11239-020-02288-0