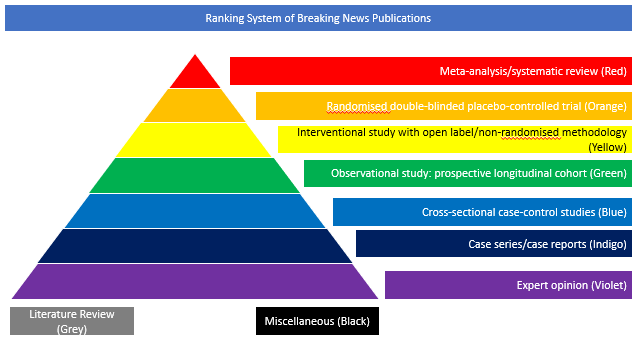
Case series/case reports (Indigo)
The objective of this article recently published in Neurology Neuroimmunology & Neuroinflammation was to investigate the pathophysiological mechanism of encephalopathy and prolonged comatose or stuporous state in severely ill patients with COVID-19. Eight COVID-19 patients with signs of encephalopathy were tested for antibodies to SARS-CoV-2 in the serum and CSF using a Food and Drug Administration-approved and independently validated ELISA. Blood-brain barrier (BBB) integrity and immunoglobulin G (IgG) intrathecal synthesis were further tested using albumin and IgG indices. The CSF was also tested for autoimmune encephalitis antibodies and 14-3-3, a marker of ongoing neurodegeneration. The authors found that all patients had anti–SARS-CoV-2 antibodies in their CSF, and 4 of 8 patients had high titres, comparable to high serum values. One patient had anti–SARS-CoV-2 IgG intrathecal synthesis, and 3 others had disruption of the blood-brain barrier. The CSF in 4 patients was positive for 14-3-3-protein suggesting ongoing neurodegeneration. In all patients, the CSF was negative for autoimmune encephalitis antibodies and SARS-CoV-2 by PCR. None of the patients, apart from persistent encephalopathic signs, had any focal neurologic signs or history of specific neurological disease. The authors concluded that high-titre anti-SARS-CoV-2 antibodies were detected in the CSF of comatose or encephalopathic patients demonstrating intrathecal IgG synthesis or BBB disruption. A disrupted BBB may facilitate the entry of cytokines and inflammatory mediators into the CNS enhancing neuroinflammation and neurodegeneration. They underlined that these observations highlight the need for prospective CSF studies to determine the pathogenic role of anti–SARS-CoV-2 antibodies and identify early therapeutic interventions.
DOI: https://doi.org/10.1212/NXI.0000000000000893