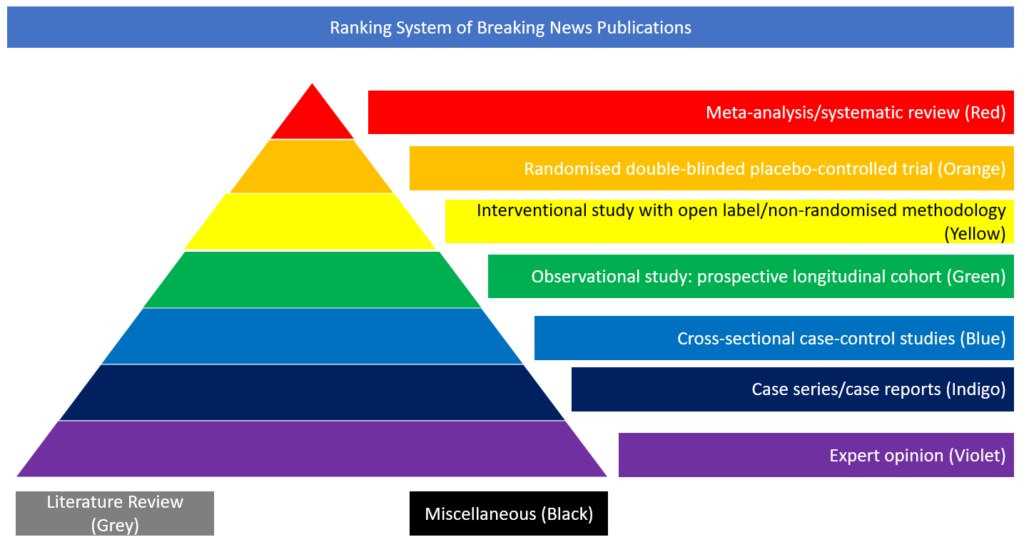
Case series/case reports
The objective of this multicentre cohort study, recently published in JAMA Internal Medicine, was to assess factors associated with death and to examine inter-hospital variation in treatment and outcomes for patients with COVID-19.
The primary outcome was 28-day in-hospital mortality. A total of 2215 patients were included in the study. At 28 days after ICU admission, 784 patients (35.4%) had died, 824 (37.2%) were discharged, and 607 (27.4%) remained hospitalised. At the end of study follow-up (median 16 days; interquartile range 8-28 days), 875 patients (39.5%) had died, 1203 (54.3%) were discharged, and 137 (6.2%) remained hospitalised. Factors independently associated with death included older age, male sex, higher body mass index, coronary artery disease, active cancer, and the presence of hypoxaemia, liver dysfunction, and kidney dysfunction at ICU admission. Patients admitted to hospitals with fewer ICU beds had a higher risk of death. Hospitals varied considerably in the risk-adjusted proportion of patients who died (range, 6.6%-80.8%) and in the percentage of patients who received hydroxychloroquine, tocilizumab, and other treatments and supportive therapies.
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2768602