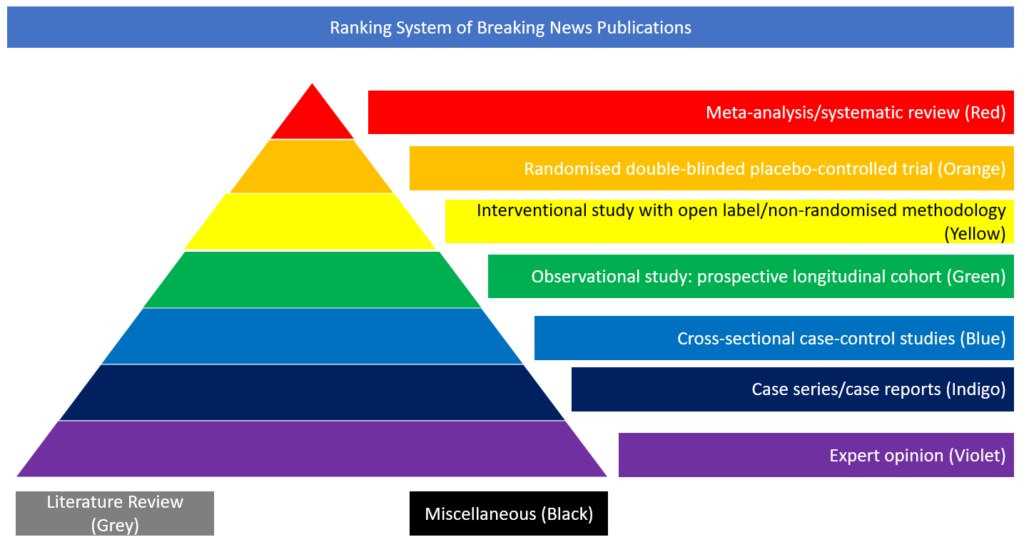
Cross-sectional case-control studies
In this paper, the authors pooled all consecutive patients hospitalised with laboratory-confirmed COVID-19 and acute ischaemic stroke across 28 sites from 16 countries.
To assess whether stroke severity and outcomes (assessed at discharge or at the latest assessment for those patients still hospitalised) in patients with acute ischaemic stroke were different between patients with COVID-19 and non-COVID-19, they performed 1:1 propensity score matching analyses. COVID-19 patients and non-COVID-19 patients registered in the Acute Stroke Registry and Analysis of Lausanne Registry between 2003 and 2019 were assessed. Between January 27, 2020, and May 19, 2020, 174 patients (median age 71.2 years; 37.9% females) with COVID-19 and acute ischaemic stroke were hospitalised. The median NIHSS score was 10 ([IQR], 4–18). In the 1:1 matched sample of 336 patients with COVID-19 and non- COVID-19, median NIHSS was higher in patients with COVID-19 (10 [IQR, 4–18] versus 6 [IQR, 3–14]), p=0.03; (odds ratio, 1.69 [95% CI, 1.08–2.65] for higher NIHSS). There were 48 (27.6%) deaths, of which 22 were attributed to COVID-19 and 26 to stroke. Among 96 survivors with available information about disability status, 49 (51%) had severe disability at discharge. In the propensity score-matched population (n=330), patients with COVID-19 had higher risk for severe disability (median mRS 4 [IQR, 2–6] versus 2 [IQR, 1–4], P<0.001) and death (odds ratio, 4.3 [95% CI, 2.22–8.30]) compared with patients without COVID-19. The authors concluded that these findings suggest that COVID-19 associated ischaemic strokes are more severe with worse functional outcome and higher mortality than non-COVID-19 ischemic strokes.
https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.031208