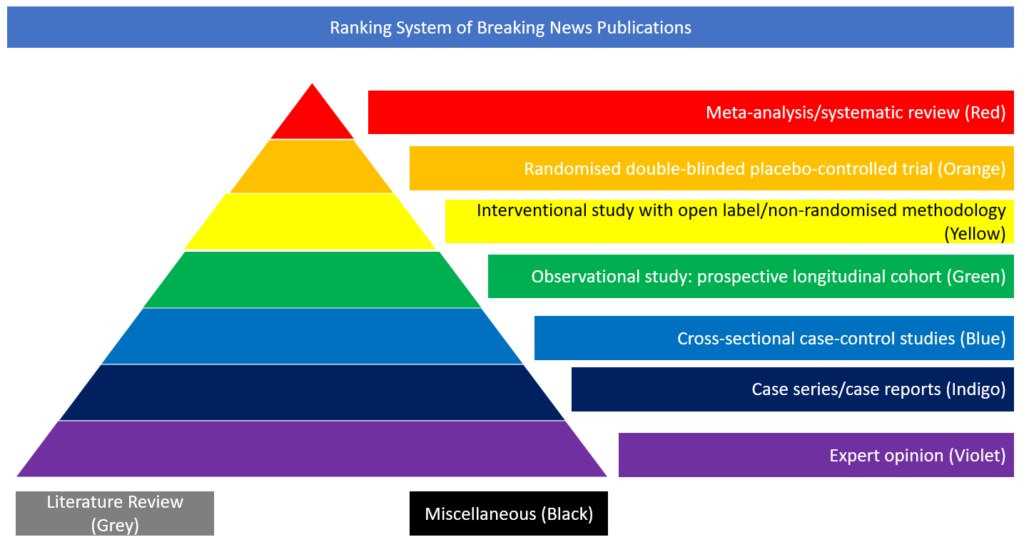
Case series/case reports
In this study, recently published in Brain, the authors present cerebrovascular disease case incidence in hospitalised patients with SARS-CoV-2 infection.
Available data on comorbidity, laboratory parameters, treatment administered, neuroimaging, neuropathological studies and clinical evolution during hospitalisation, measured by the modified Rankin scale, were analysed. A bivariate study was also designed to identify differences between ischaemic and haemorrhagic subtypes. A statistical model of binary logistic regression and sensitivity analysis was designed to study the influence of independent variables on prognosis. From 1683 admissions of patients with COVID- 19 over 50 days, 23 (1.4%) developed cerebrovascular disease. Seventeen patients were classified as cerebral ischaemia (73.9%, including two arterial dissections), five as intracerebral haemorrhage (21.7%), and one leukoencephalopathy of posterior reversible encephalopathy type. Haemorrhagic patients had higher ferritin levels at the time of stroke (1554.3 versus 519.2, p=0.004). Ischaemic strokes were unexpectedly more frequent in the vertebrobasilar territory (6/17, 35.3%). In the haemorrhagic group, a characteristic radiological pattern was identified showing subarachnoid haemorrhage, parieto-occipital leukoencephalopathy, microbleeds and single or multiple focal haematomas. Brain biopsies showed signs of thrombotic microangiopathy and endothelial injury, with no evidence of vasculitis or necrotising encephalitis. The functional prognosis during the hospital period was unfavourable in 73.9% (17/23 modified Rankin scale 4–6), and age was the main predictive variable for a poor prognosis (odds ratio = 1.5; 95% confidence interval 1.012–2.225; p=0.043). This series shows that cerebrovascular disease in patients with COVID- 19 has high morbidity and mortality. Pathological and radiological data were consistent with thrombotic microangiopathy caused by endotheliopathy with a haemorrhagic predisposition.
https://academic.oup.com/brain/article/doi/10.1093/brain/awaa239/5869424