3. Other Interventional Study Methodology
In this open-label, multicentre, randomised clinical trial, recently published in JAMA, the authors evaluate the efficacy and adverse effects of convalescent plasma therapy for patients with COVID-19. The trial included 103 participants with laboratory- confirmed COVID-19 that was severe (respiratory distress and/or hypoxaemia) or life-threatening (shock, organ failure, or requiring mechanical ventilation). The trial was terminated early after 103 from a planned 200 patients were enrolled.
Convalescent plasma in addition to standard treatment (n = 52) was compared with standard treatment alone (control) (n = 51), stratified by disease severity. Primary outcome was time to clinical improvement within 28 days, defined as patient discharged alive or reduction of 2 points on a 6-point disease severity scale (ranging from 1 [discharge] to 6 [death]). Secondary outcomes included 28-day mortality, time to discharge, and the rate of viral polymerase chain reaction (PCR) results changing from positive at baseline to negative at up to 72 hours. Of 103 patients who were randomised, 101 (98.1%) completed the trial. Clinical improvement occurred within 28 days in 51.9% (27/52) of the convalescent plasma group vs 43.1% (22/51) in the control group (difference 8.8% [95% CI −10.4% to 28.0%]; hazard ratio [HR], 1.40 [95% CI 0.79-2.49]; P = 0.26). Among those with severe disease, the primary outcome occurred in 91.3% (21/23) of the convalescent plasma group vs 68.2% (15/22) of the control group (HR 2.15 [95% CI 1.07-4.32]; P = 0.03); among those with life-threatening disease the primary outcome occurred in 20.7% (6/29) of the convalescent plasma group vs 24.1% (7/29) of the control group (HR 0.88 [95% CI 0.30-2.63]; P = 0.83) (P for interaction = 0.17). There was no significant difference in 28-day mortality (15.7% vs 24.0%; OR 0.65 [95% CI 0.29-1.46]; P = 0.30) or time from randomisation to discharge (51.0% vs 36.0% discharged by day 28; HR 1.61 [95% CI 0.88-2.93]; P = 0.12). Convalescent plasma treatment was associated with a negative conversion rate of viral PCR at 72 hours in 87.2% of the convalescent plasma group vs 37.5% of the control group (OR 11.39 [95% CI, 3.91-33.18]; P < 0.001). Two patients in the convalescent plasma group experienced adverse events within hours after transfusion that improved with supportive care. The authors concluded that, among patients with severe or life-threatening COVID-19, convalescent plasma therapy added to standard treatment, compared with standard treatment alone, did not result in a statistically significant improvement in time to clinical improvement within 28 days. Interpretation is limited by early termination of the trial, which may have been underpowered to detect a clinically important difference.
View Article: https://jamanetwork.com/journals/jama/article-abstract/2766943
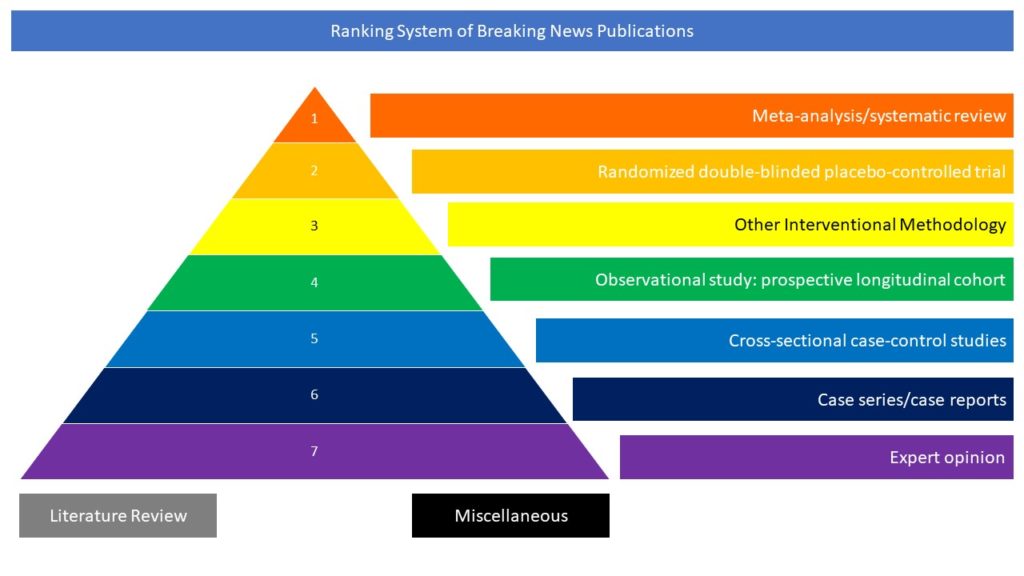
Ranking System of Breaking News Publications