by Vanja Basic Kes and Vida Demarin
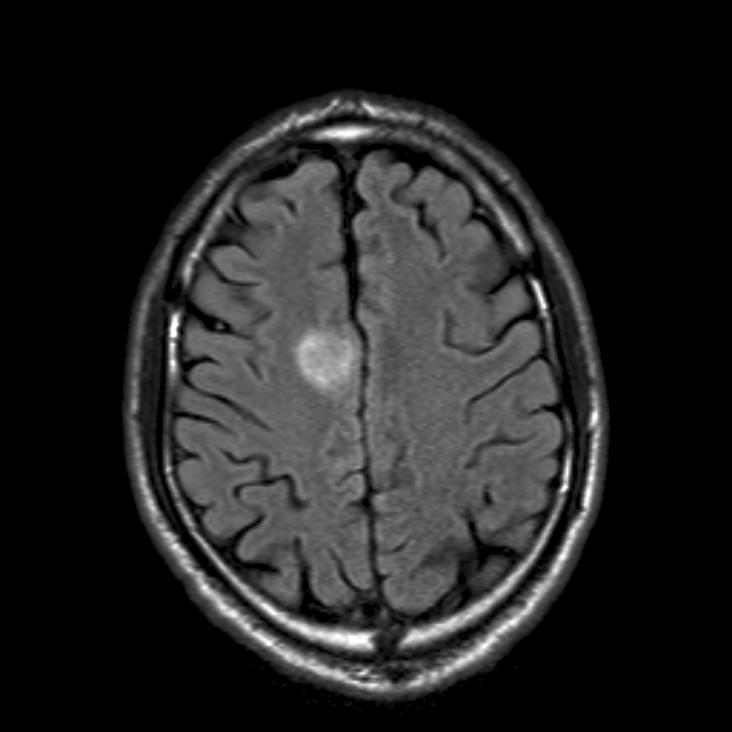
A 25-year-old female patient was admitted to our department because of deterioration of consciousness and showing verified intracerebral haemorrhagic zones on both sides of the brain on MSCT. (Figure 1)
At admission she was somnolent, out of verbal contact, had difficulties opening her eyes; orders could not be followed. All passively lifted limbs fell loosely back. At a rougher stimulus she pulled her lower extremities minimally. The tendon reflexes were facilitated and Babinski’s sign was positive on the right side. Her medical history revealed that one month ago she had been observed by a psychiatrist because of forced thoughts and panic attacks. Shortly after that she developed acute psychotic decompensation and was admitted to a psychiatric department. During the hospitalisation psychotic symptoms remained despite therapy. From the beginning of psychiatric hospitalisation she was incontinent and on the 10th day she became subfebrile. MSCT of the brain and lumbar puncture were performed but all findings were normal. The patient was transferred to the Department of Internal medicine where a neurologist was consulted. EEG was performed and showed slow brain activity. Lumbar puncture was repeated and haemorrhagic cerebrospinal fluid was found. The laboratory test excluded viral meningoencephalitis. Control MSCT and MRI of the brain were performed and revealed bilateral intracerebral haemorrhage. The consulted neurologist indicated transfer to our (neurological) department.
During hospitalisation we performed MRI and MR phlebography (Figure 2 and 3) that showed the expected dynamics of the resorptive intracerebral haemorrhage, frontoparietal and bilateral thrombosis of Trolard’s and cortical cerebral veins with still preserved blood circulation in the venous sinuses. The findings of the control MSCT of the brain showed regression of the bilateral parietal haematoma entirely to the left and a smaller bleeding residue on the right with hypodensity areas of oedema and ischemia bilaterally frontoparietal. (Figure 4)
Because of the cerebral venous thrombosis as well as proven deep vein thrombosis in the pelvic arteries and veins of the lower extremities, the blood samples were analysed for co-agulation, inflammatory and immunological tests. All of the submitted tests were normal.
Oral contraceptives which our patient took until hospitalisation at the psychiatric department seem to be the only answer to the development of disease with such unusual clinical picture.
Vanja Basic Kes is working at the Department of Neurology, University Clinical Hospital “Sestre Milosrdnice” in Zagreb, Serbia.
Vida Demarin is Professor of Neurology in Zagreb, Serbia.
Comment and questions by Adam Kobayashi
Cerebral venous thrombosis (CVT) can cause a number of sudden non-specific symptoms. Psychiatric symptoms are rather rare in this condition; and as they can be caused by a large number of other causes are rarely perceived as a symptom of CVT. This case shows how difficult it can be to diagnose such a patient unless other signs occur.
Could the authors be more specific about which tests were performed for this patient?
How was the patient treated?
Was an angio follow-up performed after treatment?
Did recanalisation occurr?
Adam Kobayashi is working at the 2nd Department of Neurology at the Institute of Psychiatry and Neurology in Warsaw, Poland. He is Secretary of the EFNS Scientist Panel Stroke.









2 comments
Did you consider a paraneoplasic origin for this systemic prothrombotic syndrome? Ovarian, breast, colon, and lung cancers are known for this rare complication.
From authors: We performed blood studies to determine prothromobotic factors such as antithrombin III, protein C or S deficiency, antiphospholipid syndrom and others. Also we searched for paraneoplastic antibodies ( anti Yo, anti Hu, anto Ro). All performed test were negative. In the beginning patient was treated with full dose of low molecular weight heparin, and after improvement, LWH was switched to oral anticoagulation therapy. Unfortunatly, the patient was lost in follow up.