by Vanja Basic Kes and Vida Demarin
A 46-year-old male was admitted to hospital one month after he had experienced pain in the right side of the neck. Some days later he had noticed choreatic movements of his left arm. He had no history of recent trauma. Clinical neurological status revealed choreatic movements of the left arm, dysarthria, gait disturbance and psychomotor restlessness. The findings of Huntington’s chorea tests and Wilson’s disease tests were normal. MSCT scan of the brain showed signs of older infarction leasons in the right n. caudatus and calcifications in both globi pallidi (Figure 1). Extracranial colour coded sonography of the right carotid artery showed a hypoechogenic area within the proximal part of the artery lumen; and absence of color-coded blood flow presumed to be a haematoma (Figure 2). The distal part revealed double lumen of the vessel with «blunted» haemodynamics in real lumen and reversed blood flow in false lumen. Left carotid artery was sub-totally stenosed (Figure 3). MSCT angiography and DSA demonstrated almost total occlusion of the right internal carotid artery and double lumen of left internal carotid artery as a sign of dissection (Figure 4).
Transcranial sonographic examination of brain parenchyma (TCS) recorded hyperechogenicity of basal ganglia (nucleus caudatus) and nuclei raphe (Figure 5).
Anticoagulation therapy with subcutaneous low molecular heparin was administered. On the 8th day the intensity and frequency of choreatic movements was reduced and on the 10th day they ceased completely. The subtotal stenosis of the left internal carotid artery was successfully operated three months later.
Further follow up for 10 months showed no relapses of extrapyramidal movements.
Spontaneous arterial dissection is a recognized cause of stroke in young patients. Usually it is associated with cerebral vascular infarction along the anterior and middle cerebral distribution. Onset of extrapyramidal movements following stroke is very rare and only a few cases are described in children.
By presenting this patient, we would like to bring to attention that sudden onset of choreatic movements may have a vascular origin, one of which is carotid artery dissection.
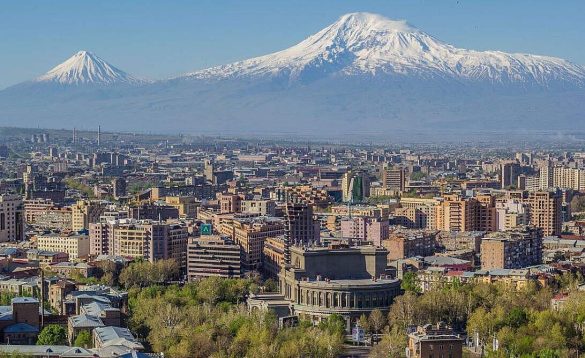
Vanja Basic Kes is Head of the Department of Neurology at the University Hospital of University Hospital Centre “Sestre milosrdnice” Zagreb, Croatia.
Comment by Michael Brainin
The case presented by Vanja Basic Kes and Vida Demarin from Zagreb, Croatia, is a rare but well documented case of transient hemichorea in contralateral spontaneous arterial dissection of the carotid artery. The patient reported to have shown choreatic movements of his left arm but also dysarthria and disturbance of gait. Within ten days the choreatic movements ceased without specific treatment. The authors present one rare but important cause of sudden onset hemi choreatic movement of vascular origin which is an important differential diagnosis of choreatic movement disorders. The sudden onset points to a possible vascular cause as does the regional limitation to one extremity or one half side of the body.
Several cases have been previously documented and there is neuropathological evidence from single case reports. The most constant location in the brain to produce extrapyramidal hyperkinetic movements is the subthalamic region and it was Malcom B. Carpenter who already produced such experimental lesions in monkeys in the early 50s. More often such lesions produce hemiballistic rather than choreatic movements, although a mix of both may be present. Further cases are documented in J.P. Mohr’s Stroke Textbook. JP Mohr reports that hemichorea – hemiballismus are the most common documented forms of movement disorder accounting for 2/3 of a series of 22 patients investigated for movement disorders of vascular origin. Of these lacunar infarcts are the most frequent cause. These can be located in different parts of the striatum, the head of the caudate nucleus and adjacent corona radiata, the subthalamic nucleus and the thalamus. Usually the disturbance is transient but it may also fluctuate in some rare instances. Treatment with haloperidol is a common approach but experience with newer neuroleptics has not been reported. The hemichorea – hemiballismus type of hyperkinetic movement disorder must be differentiated from dystonia.
Two types of dystonia can occur in the presence of acute lacunes. One is action induced rhythmic dystonia which erupts when voluntary movements of any part of the body including even eye-closure can precipitate rhythmic dystonic extension and rotation of the arm and leg usually of short duration such as for several seconds. The other type is focal dystonia where the movements are slower, causing the patients fingers to assume unusual positions and postures, typically with hyperpronation and flexion at the wrist. While action induced rhythmic dystonia maybe more responsive to clonazepam focal dystonia might cease more easily with neuroleptic therapy. The described movement disorders have to be differentiated from other involuntary movement disorders associated with vascular lesions such as asterixis (unilateral flapping tremor) or unilateral tremor that can appear several months after lacunar infarction.
In sum this case report from our Croatian colleagues is noteworthy not only due to its rare clinical phenomenology but especially for its etiology. Now carotid dissection has to be added to the list of causes for sudden onset hemichorea of vascular origin.
Recommended reading:
Carpenter MB. Human Neuroanatomy. 7th Edition (1976) Williams and Wilkins. Baltimore. 1976
Mohr JP, Wolf PA, Grotta JC, et al. Stroke. 5th Edition. Elsevier New York 2011, 499 – 500
Micheal Brainin is Professor of Neurology and Head of the Centre of Neuroscience at the Donau University in Krems, Austria. He is chairperson of the EFNS Scientific Committee.