by Euphrosyni Koutsouraki et al.
Demyelination in white matter tracts has been observed in experimental and human spinal cord injury but the precise pathophysiologic mechanisms still remain a matter of speculation. The cellular inflammatory response induced by spinal trauma is comprised of microglia, astrocytes, infiltrating neutrophils, monocytes, and activated lymphocytes against a variety of antigens, including myelin basic protein. Post-traumatic myelopathy commonly mimics multiple sclerosis (MS) and neuromyelitis optica (NMO) without clear differential diagnostic criteria between these three diseases.
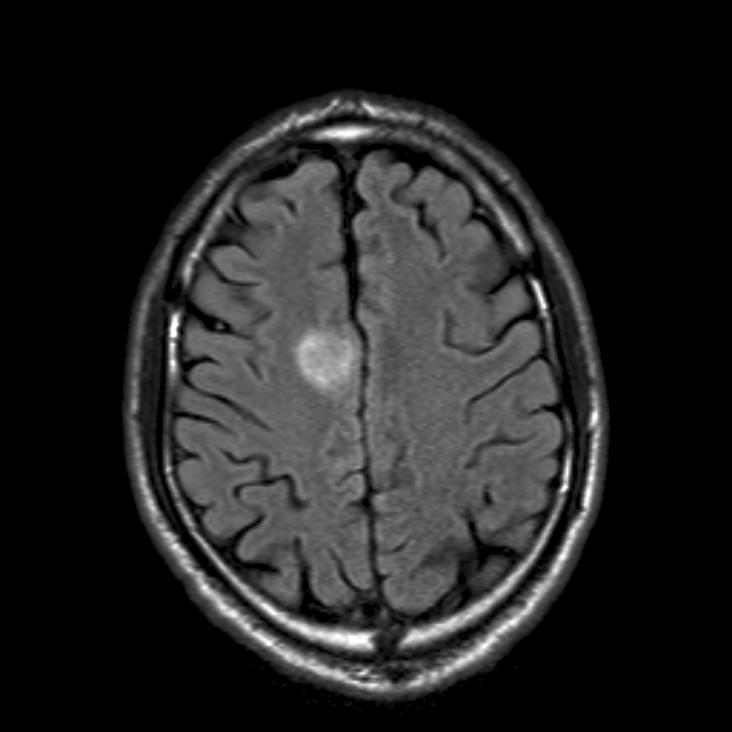
We present the case of a middle-aged Caucasian female who developed progressive spastic quatraparesis, more severe in the lower limbs, atrophies in her hands, visual impairment and sphincter dysfunction, throughout a two-year period after a cranio-cervical trauma. Magnetic Resonance Imaging (MRI) examinations revealed extensive demyelinating lesions in the cervical spinal cord without any further central nervous system (CNS) lesions. Neurophysiological investigations indicated lesions of the pyramidal tracts, the anterior horns of the spinal cord as well as important dysfunction of the visual tract. Anti-aquaporin-4 was negative and the cerebrospinal fluid analysis showed oligoclonal IgG bands. For the last six years the neurological status of the patient has remained stable with symptomatic treatment. The patient is currently treated with immunosuppressant drugs (Azathioprine and corticosteroids) and demonstrated great improvement with corticosteroid therapy.
We believe that this is a probable case of an auto-immune, post-traumatic, demyelinating myelopathy mimicking late-onset primary progressive, spinal type, MS. Post-traumatic demyelination in the spinal cord should be investigated in more detail as a possible contributor to chronic deficits and one should define the nature, time of occurrence, and proportional significance of secondary damage in order to differentiate acute secondary pathophysiology from primary degenerative processes. It is also very important to differentiate the post-traumatic demyelination from MS and NMO triggered by a trauma.
E. Koutsouraki, A. Kiryttopoulos, Th. Kalatha, A. Fotakidou, M. Arnaoutoglou, A. Orologas are working at the 1st Department of Neurology, Aristotle University, AHEPA Hospital, Thessaloniki, Greece.
Comment by Ralf Gold
The authors describe an interesting case of cervical myelitis and neuronopathy, in possible conjunction with preceding cervical trauma. Also the optic nerves were afflicted, yet aquaporin antibodies were negative.
Is this a variant of neuromyelitis or true trauma-activated inflammation? All of us know patients who link their first relapse of MS with physical over-activity, infection, military service or other stressful events. In expert opinion statements this is usually NOT regarded as sufficient for initiation of a chronic autoimmune process, an important consideration for handling insurance cases. On the other hand experimental studies of the 1990s clearly showed that a mechanical brain lesion became a target for subsequent experimental encephalomyelitis, when this was induced by immunisation.
Currently we have no tools to differentiate whether trauma just activated a smouldering process in the spinal cord, or was the key event for starting an avalanche of immuno-inflammatory processes. Regardless what came first, this patient needs proper treatment for the autoimmune process. As a devil’s advocate one may discuss that the combination of azathioprine and steroids is also appropriate in milder variants of NMO.
Ralf Gold is Professor of Neurology at the Ruhr-University Bochum, Germany and Chairperson of the EFNS Scientist Panel Demyelinating Diseases.




1 comment
Thanks for the excellent case. But milder form of Adrenomyeloneuropathy in a female carrier should come in D/D as it is a curable condition.